Thoracic surgery- a branch of medicine that deals mainly with the surgical treatment of organ diseases chest– lungs, pleura, mediastinum and others.
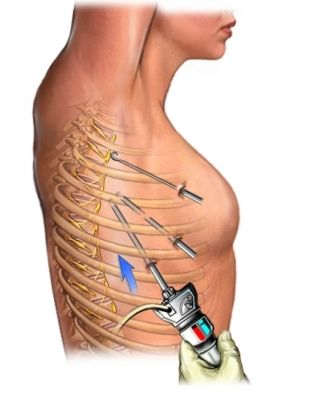
At different times, at different years thoracic surgeons performed surgery on the breast, lungs, heart, esophagus, and mediastinum. Exactly from thoracic surgery such modern areas as cardiac surgery, mammology, and angiosurgery emerged. At today's technological level of development of medicine, there is again a tendency towards convergence of all these disciplines. This can be seen both in domestic clinics and abroad. The reason is new technical capabilities. For example, many operations can now be done using a thoracoscope (endoscope for the chest cavity). Its illuminated optical system allows operations without large incisions. The surgeon sees his own actions on the monitor. Even a tumor can be removed through incisions of 3-4 cm. Thanks to minimally invasive technologies developed by thoracic surgeons (videothoracoscopy, mediastinoscopy), qualitatively new possibilities for operating on the lungs, heart, and mediastinum have emerged. A number of operations on the nerve trunks, which were forgotten due to the traumatic nature, have been revived, diagnostic capabilities have been expanded by obtaining tissue samples for histological examination, and hours-long operations accompanied by multi-liter blood losses and gross cosmetic defects have become a thing of the past.
Thoracic surgeon– specialist in chest and mediastinal surgery. From Greek thorax - chest. A thoracic surgeon is a specialist in the surgical (using operations) treatment of the chest and mediastinal organs.
Features of the profession
Thoracic (also known as thoracic) surgery deals with the surgical treatment of the lungs and pleura, mediastinum and other organs of the chest.
The work of a thoracic surgeon is often associated with pulmonology and phthisiology. It is no coincidence that thoracic surgeons work in tuberculosis dispensaries. But even from the definition it is clear that this profession is somewhat broader.
A thoracic surgeon can treat injuries (including penetrating ones) of the chest and hidden organs (including the heart), inflammation of the sternum and ribs, tumors of the lungs, chest, thyroid gland, etc., ruptures of the lung, esophagus, diaphragm, etc. P.
Important qualities
The profession of a thoracic surgeon presupposes such qualities as responsibility, good intelligence and a tendency to self-education, and self-confidence. A surgeon's determination will be of no use unless it is combined with a kind and responsible attitude towards patients. An aptitude for working with your hands and good motor skills are also required. Calm attitude towards the sight of blood.
Knowledge and skills
In addition to anatomy, physiology and other general medical disciplines, thoracic surgeon must thoroughly know the physiology of the chest and mediastinal organs, master diagnostic methods, conservative and surgical treatment, perform operations and other medical procedures (bandaging, suturing, tracheostomy, etc., etc.).
The illustration shows the chest and mediastinum in cross section.
Thorax (lat. thorax)- part of the body formed by the sternum, ribs, spine and muscles.
Inside it is the thoracic cavity and the diaphragm (curved top part abdominal cavity).
Mediastinum– part of the chest cavity above the diaphragm between the sternum and the spine. The mediastinum contains the heart and pericardium, large vessels and nerves, the trachea and main bronchi, the esophagus, and the thoracic duct.
Mediastinal tumors
The problem of diagnosis and treatment of mediastinal tumors still remains the most complex and relevant in clinical oncology. These neoplasms account for 2-7% of all human tumors. IN initial stages Mediastinal tumors are asymptomatic or with minor organ-specific symptoms. In 1/3 of patients there are no clinical symptoms. As the tumor size increases, pressure, displacement and invasion into adjacent structures and organs, mediastinal syndromes develop. Despite the expansion of the possibilities of primary and clarifying diagnostics, methods of morphological verification of the tumor, establishing an accurate diagnosis sometimes remains a difficult task for the clinician.
The choice of optimal treatment tactics often causes significant difficulties due to the variety of histological forms of neoplasms, the peculiarities of their localization in various parts of the mediastinum and relationships with neighboring anatomical structures and organs.
Tracheal tumors
Malignant tumors of the trachea are divided into primary and secondary. Primary ones develop from the wall of the trachea, secondary ones are the growth of malignant tumors of neighboring organs into the trachea: larynx, thyroid gland, lung and bronchi, esophagus, lymph nodes, mediastinum. Primary make up 0.1-0.2% of all malignant neoplasms. The most common histological forms are adenoid cystic carcinoma (cylindroma) and squamous cell carcinoma, accounting for 75-90% of all malignant tracheal tumors. Primary tracheal tumors occur more often in men than in women, mainly between the ages of 20 and 60 years.
Malignant tumors of the trachea manifest themselves as a characteristic symptom of difficulty breathing - shortness of breath and even stridor (a whistling noise caused by a sharp narrowing of the tracheal lumen. Shortness of breath usually increases gradually, but always noticeably intensifies with physical activity(fast walking, climbing stairs, sometimes even while talking).
Diagnosis: based on complaints, medical history, assessment of the patient’s condition, but most importantly - on data from special research methods.
Lung tumors
The mortality rate from this malignant lung tumor reaches 85% of all patients, despite modern advances in medicine. In some countries, lung cancer is also beginning to take first place in morbidity and mortality among women. The main cause of lung cancer is smoking. About 80% of patients with this pathology are smokers. The remaining 20% of cancer cases are associated with exposure factors such as indoor radon, contact with asbestos dust, heavy metals, and chlormethyl ether.
Clinical manifestations: cough, shortness of breath, chest pain, hemoptysis, weight loss.
If you have any complaints, you should immediately consult a doctor.
Esophageal tumors
Among all malignant tumors of the digestive tract, esophageal cancer ranks third after stomach and rectal cancer. Unfortunately, severe symptoms appear at fairly late stages and a relatively small percentage of patients can be treated radically. At least 80% of patients are hospitalized already at stages III-IV of the disease.
Risk factors for the development of esophageal cancer are recognized as systematic contact with carcinogenic substances, chronic radiation exposure, excessive mechanical, thermal, chemical irritation of the esophageal mucosa, cicatricial narrowing of the esophagus after chemical burns, its achalasia, hiatal hernia, reflux esophagitis.
“Alarm signals” that suggest the possibility of a malignant neoplasm of the esophagus are:
dysphagia (impaired swallowing) of any severity, occurring regardless of mechanical, thermal or chemical injury to the esophagus;
sensation of passing a bolus of food, pain or discomfort along the esophagus, arising when eating;
repeated regurgitation (regurgitation of food) or vomiting, especially with blood;
Hoarseness that appeared for no reason.
Instrumental research methods are crucial in recognizing esophageal cancer - these are x-ray and endoscopic examinations.
Treatment of patients with esophageal cancer is one of the most challenging tasks in clinical oncology. Surgical, radiation and combined methods are used. Surgical treatment of esophageal cancer consists of subtotal resection or extirpation and subsequent plastic surgery with a gastric, small- or colonic graft.
A thoracic surgeon is a physician responsible for treating the thoracic organs (diaphragm, lungs, breast, heart, esophagus and others). Today, taking into account the peculiarities of thoracic surgery, professionals in this field work in more narrow specializations: mammology, cardiology and pulmonology. The vital organs for which people seek help from such doctors are the lungs and heart.
What does a thoracic surgeon treat?
Most often, according to statistics, doctors of this surgery encounter such complications and diseases as:
- ailments of blood vessels and heart;
- cystic formations and tumors of the chest organs:
- diseases of the bronchi and lungs (emphysema, purulent-inflammatory developments, ulcers);
- pathologies of the thymus and thyroid glands;
- diseases of the mediastinum;
- vomiting, heartburn, hiccups and belching;
- burns, inflammation of the lining of the esophagus.
The scope of work of a thoracic surgeon also includes the removal of foreign objects from the esophagus and various other injuries to the thoracic region.

What organs does a doctor deal with?
Many people already know who a thoracic surgeon is. What exactly does it treat? The list of organs is far from small:
- large lymphatic and blood vessels;
- parathyroid and thyroid glands;
- larynx;
- pericardium;
- esophagus;
- lungs;
- pharynx;
- heart;
- stomach;
- diaphragm;
- thymus (thymus gland);
- liver.
Indicators of esophageal disorders
Manifestations of esophageal dysfunction include:
- vomiting and hiccups;
- belching and heartburn;
- odynophagia (pain when food passes through the esophagus);
- dysphagia (disorder of passage of food through the esophagus);
- pain in the esophagus and epigastrium (“in the pit of the stomach”);
- feeling of a lump behind the chest.

What indicators does thymus cancer have?
There are no clinical symptoms of such cancer in the early stages of the disease. When the tumor puts pressure on nearby organs, breathing problems may occur, difficulty in the flow and outflow of blood from the external vena cava (headaches, blue discoloration and swelling upper limbs, face, increased intracranial pressure), heart rhythm disorder.
Main types of diagnostics
A thoracic surgeon usually performs some types of research, namely:
- biopsy;
- arthroscopy;
- hysteroscopy;
- thoracoscopy;
- laparoscopy;
- thoracoscopic removal of focal lung diseases limited by the method of preoperative contrast;
- video thoracoscopic thymectomy;
- video thoracoscopic pleurodesis in the treatment of substandard exudative pleuritis;
- videothoracoscopy for initial ailments of the mediastinal organs;
- intraoperative examination during the period of thoracoscopic measures regarding focal lung diseases.
Necessary tests
The thoracic surgeon, first of all, always prescribes certain tests:
- urine;
- blood;
- for HIV;
- drug allergy test.

For lung and chest injuries, a specialist can give specific instructions on how to provide first aid.
- The victim should be seated comfortably.
- Apply cold to the damaged area.
- If there is a wound, you need to disinfect the area with iodine and cover it with a sterile bandage. If the chest is damaged at the location of the wound, a whistling sound is heard when exhaling and inhaling. Along with the escaping air, bloody clots come out of the wound. The thoracic surgeon advises applying polyethylene or other airtight material to the wound. This can be done with strips of adhesive tape or a bandage.
- It is better to bring the victim to the clinic as quickly as possible and preferably in a sitting position.
Surgical methods
Certain types of operations are performed in specialized medical institutions. A consultation with a thoracic surgeon will help you become more familiar with these surgical types. Here are some of them:
- complex reconstructive plastic resections of the lungs for cancerous lesions with connecting operations of the chest membrane, large vessels, trachea, heart, bronchi, diaphragm;
- removal of the trachea in case of scar or tumor damage;
- operations for diseases of the septum, also with resection of the diaphragm, lung, heart and great vessels;
- surgical interventions for anomalies of the thymus gland and myasthenia;
- resection for ailments of the diaphragm and hernia of its food passage;
- operations in the thoracic region for acute, persistent purulent-inflammatory diseases of the pleura, ribs and chest;
- the thoracic surgeon also performs video-assisted thoracoscopic resections on the esophagus, mediastinum, trachea, lungs, bronchi, including the removal of foreign materials;
- operations for thoracotrauma, wounds of the neck, sternum, and heart;
- resections on the thyroid gland.
Head of department
- “The Department of Thoracic Surgery was founded in 1968 on the initiative of the greatest pediatric surgeon of his time, Academician of the Russian Academy of Medical Sciences, Head. Department of Pediatric Surgery of the Central Institute for Advanced Medical Studies, the founder of the school of pediatric surgery, widely known both in the USSR and abroad, by Professor Stanislav Yakovlevich Doletsky. Professors V.A. Timoschenko, V.E. Shchitinin, V.G. made a great contribution to the formation of the school of thoracic surgery. Geld."
Currently, the department has 30 clinical beds. Every year, up to 700 children undergo treatment across the entire spectrum, both emergency and planned thoracic pathologies, and about a thousand different operations and specialized manipulations are performed.
Congenital and acquired diseases of the trachea: congenital and cicatricial stenoses, tracheoesophageal fistulas, cystic duplications, etc.
Tumors and cysts of the neck (lateral, median and lymph and hemangiomas...)
Congenital and acquired diseases of the esophagus: stenosis of any etiology, duplication, gastroesophageal reflux disease, recanalization of tracheoesophageal fistula in children operated on for fistulous forms of esophageal atresia, etc.
Malformations of the diaphragm: true and false diaphragmatic hernias, hiatal hernias, traumatic diaphragmatic hernias.
All types of chest deformities: pectus excavatum, carinatum, cleft sternum, Luschke's rib, syndromic forms, postoperative (secondary) deformities.
Modern equipment, progressive methods of treatment and operational aids make it possible to provide assistance to children who come with relapses of diseases after providing them with medical care in other medical institutions.
The department is equipped with the most modern intraluminal endoscopic and endosurgical equipment, which annually conducts more than 600 endoscopic examinations of children with thoracic pathology - laryngo, tracheo- and bronchoscopy, esophagogastroduodenoscopy, using both fiber and rigid optics. About 150 emergency patients are evaluated annually for suspected foreign bodies respiratory tract and the upper gastrointestinal tract, up to 50-70 different foreign bodies are removed. More than 300 bougienages of the esophagus and trachea are performed using balloon dilatation and thermoplastic bougies. Stenting is actively used. More than 50 patients are being examined for GERD using 24-hour Ph monitoring.
Since 1985 The department of thoracic surgery began to actively introduce treatment methods using endosurgical access into practice. Today, most thoracic patients are operated on using high-tech methods, including endosurgical methods.
Department of Thoracic Surgery hospital of St. Vladimir is the base of the Department of Pediatric Surgery of the Russian Medical Academy of Postgraduate Education, where residents and graduate students of Russian universities are trained and pediatric surgeons from all regions of the country receive specialist certificates. For many years, the department has been actively collaborating with the largest institutes and clinics in Moscow and Russia (SCCH RAS, CITO named after N.N. Priorov, Sklifosovsky Institute, 1st Medical University named after I.M. Sechenov, 7DKB, 9DKB, 6KIB, 1 KIB, 2 KIB, etc.)
Every year the department publishes up to 10 works and speaks at both Russian and international forums.
Doctors of the department:
Topilin Oleg Grigorievich – thoracic surgeon of the highest qualification category. Postgraduate student of the Department of Pediatric Surgery of the Russian Medical Academy of Postgraduate Education. Author of more than 30 published works and 3 patents.
Safin Dinar Adhamovich – pediatric surgeon. Has I qualification category in pediatric surgery. In 2010, he completed his residency in pediatric surgery at the Russian Medical Academy of Postgraduate Education. Postgraduate student of the Department of Pediatric Surgery of the Russian Medical Academy of Postgraduate Education. Author of 12 published works and 1 patent for invention.
Tkachenko Nadezhda Vitalievna - pediatrician. Has the highest qualification category in pediatrics. 17 years of experience.
Dikiy Alexander Leonidovich – endoscopist. Completed primary retraining in endoscopy. Has the first qualification category in pediatric surgery. Work experience 8 years.
Senior med. sister:
Gerash Irina Anatolyevna. Work experience 15 years. Honey. sister of the 1st qualification category.
The department employs 9 guard nurses, all with the highest qualification category, a sister in the endoscopy room, a sister housewife with 23 years of experience, two barmaids and three nurses.
Most operations performed by thoracic surgeons are operations related to the treatment of chest wall and metastases in the lungs.
Thoracic surgeon - chest surgeon. The activities of these doctors extend to the chest organs and chest wall.
Surgery is performed on the lungs, trachea, bronchi, pleura and mediastinal organs. The mediastinum is the heart with the pericardial sac, large and esophagus. These vessels include the aorta with its arch, pulmonary veins, arteries, thoracic lymphatic duct and trunks of the vena cava. Also in the mediastinum there is a large number of nerve plexuses and. Due to the multitude of anatomical structures and the complexity of operations, such narrow specializations as cardiac surgeons, breast surgeons and vascular surgeons emerged from this branch of medicine.
Chest injuries, for example:
- hemothorax (accumulation of blood in the pleural cavity)
- chylothorax (lymph in the pleural cavity)
- pneumothorax (penetration of air into the pleural cavity)
Clinical diagnostic methods in thoracic surgery
For a successful operation, the doctor must conduct a complete diagnosis. It all starts with collecting an anamnesis - a survey, and a physical examination - percussion of the chest.
- The percussion method - tapping the chest, allows you to determine by sound the type and location of some pathologies of the lungs and heart.
- X-ray examination is a classic method for examining the chest organs in thoracosurgery. The method makes it possible to diagnose lung pathologies with great accuracy, since any compaction in the lung tissue appears on an x-ray.
- Ultrasound examination () - is especially often used to diagnose pathologies and tumors in the area of the pleural sac.
- Computed tomography of the chest is indispensable in thoracic surgery; it allows you to obtain a three-dimensional image of an organ or area, giving the doctor spatial orientation, which allows you to more accurately determine the nature of the pathology and the stages of the operation.
- MRI – unlike computed tomography and x-ray examination, the magnetic resonance imaging method is absolutely safe, excluding radiation exposure to the patient. The advantage is also better visualization of soft tissues. This allows the doctor to accurately determine the location of inflammatory processes, tumor foci and other pathologies. Magnetic resonance imaging is used not only for diagnosis before surgery, but also for postoperative follow-up.
- Thoracoscopy - is endoscopic, using a laparoscope - a device in the form of a tube with a camera and a light source, equipped with a device for aspiration and rinsing. The device is inserted directly through the chest wall into the pleural cavity. The thoracoscopy method allows you to take a biopsy and operate in the pleural cavity and on the layers of the pleura, as well as on the pulmonary surfaces adjacent to the ribs.
The goal of all diagnostic manipulations is to determine the location and extent of the disease; this is the only way to competently plan the intervention and take into account possible risks.
Thoracic surgery departments in Moscow, information for patients
Departments of thoracic surgery in Moscow provide complete packages of services for the treatment of diseases of the chest cavity. Leading thoracic surgeons who are proficient in low-traumatic operating methods work in this area.
Modern equipment and infrastructure make it possible to successfully diagnose and treat diseases of the mediastinum, trachea, lungs, pericardium, chest wall and diaphragm. To ensure the least discomfort during the treatment process and provide the patient with effective postoperative treatment. Patients have the opportunity to familiarize themselves with the list of diseases that require operations in thoracic surgery departments and discuss the treatment process with a doctor.
In Moscow they provide this kind of:
- City Hospital named after. S.I. Spasokukotsky
- Department of Pediatric Thoracic Surgery named after. N.F. Filatova
- Department of Thoracic Surgery at the Russian National Medical and Surgical Center named after. Pirogov.
At the moment, in Moscow, the field of thoracic surgery is quite common and publicly available.
Sep 7, 2016 Violetta Doctor
This is a specialist whose competence includes the treatment of diseases of the chest organs. He diagnoses pathologies and performs operations on the lungs, bronchi, esophagus and mediastinum.
What does thoracic treat?
Most often, patients are admitted to the hospital with chest injuries, for example, after a traffic accident, or with advanced purulent-inflammatory processes, when for some reason the patient postponed a visit to the doctor. In their practice, these surgeons more than once encounter the treatment of tumors, malignant and benign, as well as tuberculosis.
Thoracic treats respiratory diseases such as:
- pleurisy;
- empyema of the pleural cavity (purulent accumulations);
- pericarditis;
- lung abscess (a cavity with pus is formed);
- pulmonary embolism (in other words, its blockage);
- chylothorax - when lymph accumulates in the pleural area;
- mediastinitis - inflammatory processes of mediastinal tissue; for reference: the mediastinum is the anatomical space in the middle section of the chest;
- bronchiectasis (due to damage to the bronchial wall, irreversible expansion of the bronchial tube appears);
- atelectasis (due to its collapse, air ceases to flow into a certain area of the lung, as a result of which normal gas exchange becomes impossible);
- stenosis of the bronchi and trachea (characterized by narrowing of the lumens);
- pneumothorax (including in children of the first year of life) - air accumulates between the two layers of the pleura;
- osteomyelitis - the bone tissue of the ribs becomes inflamed with the formation of pus;
- chondritis, perichondritis.
The doctor also performs surgical treatment of esophageal pathologies:
- esophagitis - the walls of the esophagus become inflamed;
- achalasia - impaired swallowing function;
- diverticula of the esophagus (when they form, the wall of the esophagus protrudes);
- fistulas and burns;
- removal of foreign objects from the esophagus;
We will especially highlight the treatment of pathologies of the thymus and thyroid glands.
When should I go for an appointment?
Usually another specialist, for example, or a therapist, refers you to a thoracic specialist. In other situations, the patient is brought in by ambulance, for example, after receiving a chest injury.
Symptoms that require you to see a doctor immediately:
- prolonged cough with pus and an unpleasant odor;
- hemoptysis;
- chest pain (the location of the pain, its increasing nature, and the time of occurrence are important: when walking, breathing, or even at rest);
- dyspnea;
- feeling of suffocation;
- dysphagia - difficulty swallowing food.
Always treats in a hospital setting. Whether and what tests will be ordered depends on the severity of the case. If the situation is not critical and time allows for tests, be sure to examine blood and urine, sputum, and take an x-ray.
Diagnostic methods used
When the operation is planned, it is possible to examine the patient comprehensively. Therefore, in addition to the above tests, the patient may be prescribed:
- ultrasonography;
- angiography (shows the condition of the vessels);
- tomography (spiral computer or positron emission tomography) - allows you to obtain a 3D image of the bronchial tree;
- thoracoscopy (examination of the pleural area);
- magnetic resonance imaging;
- pleural puncture;
- biopsy;
- interventional sonography;
- autofluorescence bronchoscopy (examination for the presence of a tumor);
- spirography (determines the vital volume of the lungs).
Modern surgical treatment involves not only the use of a scalpel, but also the use of minimally invasive intervention methods (for example, laparoscopy), microsurgical and laser technologies. Diagnostic procedures are performed in so-called hybrid operating rooms, where modern magnetic resonance imaging scanners, fixed C-arms, and angiographic equipment are installed. This helps to significantly reduce the risk of complications by making miniature incisions or punctures during surgery.
Thanks to new technologies, the patient's stay in the hospital is reduced. postoperative period, and also improves the quality of surgical treatment. This means that more than one life will be saved.