After intervention in the body of a sick patient, a postoperative period is required, which is aimed at eliminating complications and providing competent care. This process is carried out in clinics and hospitals and includes several stages of recovery. At each period, attentiveness and care for the patient on the part of the nurse, and medical supervision are required to exclude complications.
What is the postoperative period
In medical terminology, the postoperative period is the time from the end of the operation until the patient’s complete recovery. It is divided into three stages:
- early period – before discharge from hospital;
- late – after two months after surgery;
- long-term period is the final outcome of the disease.
How long does it last
End date postoperative period depends on the severity of the disease and individual characteristics the patient's body aimed at the healing process. Recovery time is divided into four phases:
- catabolic – an upward change in the excretion of nitrogenous wastes in the urine, dysproteinemia, hyperglycemia, leukocytosis, weight loss;
- period of reverse development - the influence of hypersecretion of anabolic hormones (insulin, somatotropic);
- anabolic – restoration of electrolyte, protein, carbohydrate, fat metabolism;
- period of increasing healthy body weight.
Goals and objectives
Observation after surgery is aimed at restoring normal activity of the patient. The objectives of the period are:
- prevention of complications;
- recognition of pathologies;
- patient care - administering analgesics, blockades, providing life support important functions, dressings;
- preventive measures to combat intoxication and infection.
Early postoperative period
The early postoperative period lasts from the second to the seventh day after surgery. During these days, doctors eliminate complications (pneumonia, respiratory and renal failure, jaundice, fever, thromboembolic disorders). This period affects the outcome of the operation, which depends on the state of kidney function. Early postoperative complications are almost always characterized by impaired renal function due to the redistribution of fluid in sectors of the body.
Renal blood flow decreases, which ends on days 2-3, but sometimes the pathologies are too serious - loss of fluid, vomiting, diarrhea, impaired homeostasis, acute renal failure. Protective therapy, replenishment of blood loss, electrolytes, and stimulation of diuresis help avoid complications. Common reasons The development of pathologies in the early period after surgery is considered to be shock, collapse, hemolysis, muscle damage, and burns.
Complications
Complications of the early postoperative period in patients are characterized by the following possible manifestations:
- dangerous bleeding– after operations on large vessels;
- cavity bleeding - during intervention in the abdominal or thoracic cavities;
- pallor, shortness of breath, thirst, frequent weak pulse;
- wound dehiscence, lesion internal organs;
- dynamic paralytic ileus;
- persistent vomiting;
- the possibility of peritonitis;
- purulent-septic processes, fistula formation;
- pneumonia, heart failure;
- thromboembolism, thrombophlebitis.
Late postoperative period
After 10 days from the moment of surgery, the late postoperative period begins. It is divided into hospital and home leave. The first period is characterized by an improvement in the patient’s condition and the beginning of movement around the ward. It lasts 10-14 days, after which the patient is discharged from the hospital and sent for home postoperative recovery, a diet, vitamin intake and activity restrictions are prescribed.
Complications
The following late complications after surgery are identified, which occur while the patient is at home or in the hospital:
- postoperative hernias;
- adhesive intestinal obstruction;
- fistulas;
- bronchitis, intestinal paresis;
- repeated need for surgery.
The causes of complications in later After surgery, doctors name the following factors:
- long period of stay in bed;
- initial risk factors – age, illness;
- respiratory dysfunction due to prolonged anesthesia;
- violation of the rules of asepsis for the operated patient.
Nursing care in the postoperative period
An important role in caring for the patient after surgery is played by nursing care, which continues until the patient is discharged from the department. If it is not enough or is performed poorly, this leads to unfavorable outcomes and prolongation of the recovery period. The nurse should prevent any complications, and if they occur, make efforts to eliminate them.
The duties of a nurse in postoperative patient care include the following responsibilities:
- timely administration of medications;
- patient care;
- participation in feeding;
- hygienic care of skin and oral cavity;
- monitoring for deterioration and providing first aid.
From the moment the patient enters the intensive care ward, the nurse begins to perform her duties:
- ventilate the room;
- eliminate bright light;
- position the bed for a comfortable approach to the patient;
- monitor the patient's bed rest;
- prevent cough and vomiting;
- monitor the position of the patient's head;
- feed.

How is the postoperative period going?
Depending on the patient’s condition after surgery, the stages of postoperative processes are distinguished:
- strict bed rest period - it is forbidden to get up or even turn around in bed, any manipulation is prohibited;
- bed rest - under the supervision of a nurse or exercise therapy specialist, it is allowed to turn over in bed, sit down, lower your legs;
- ward period - it is allowed to sit on a chair and walk for a short time, but examination, feeding and urination are still carried out in the ward;
- General regime – patient self-care, walking along the corridor, offices, and walks in the hospital area are allowed.
Bed rest
After the risk of complications has passed, the patient is transferred from intensive care to the ward, where he must remain in bed. The goals of bed rest are:
- limitation of physical activity, mobility;
- adaptation of the body to hypoxia syndrome;
- pain reduction;
- restoration of strength.
Bed rest is characterized by the use of functional beds, which can automatically support the patient’s position - on the back, stomach, side, half-lying, half-sitting. The nurse cares for the patient during this period - changes underwear, helps to cope with physiological needs (urination, defecation) if they are difficult, feeds and carries out hygiene procedures.
Following a special diet
The postoperative period is characterized by adherence to a special diet, which depends on the volume and nature of the surgical intervention:
- After operations on the gastrointestinal tract, enteral nutrition is provided for the first days (through a tube), then broth, jelly, and crackers are given.
- When operating on the esophagus and stomach, the first food should not be taken through the mouth for two days. Parenteral nutrition is provided - subcutaneous and intravenous administration of glucose and blood substitutes through a catheter, and nutritional enemas are performed. From the second day broths and jelly can be given, on the 4th day crackers are added, on the 6th mushy food, from 10 common table.
- In the absence of violations of the integrity of the digestive organs, broths, pureed soups, jelly, and baked apples are prescribed.
- After operations on the colon, conditions are created so that the patient does not have stool for 4-5 days. Low fiber diet.
- When operating on the oral cavity, a probe is inserted through the nose to provide liquid food.
You can start feeding patients 6-8 hours after surgery. Recommendations: maintain water-salt and protein metabolism, provide sufficient amounts of vitamins. A balanced postoperative diet for patients consists of 80-100 g of protein, 80-100 g of fat and 400-500 g of carbohydrates daily. Enteral formulas and dietary canned meat and vegetables are used for feeding.
![]()
Intensive monitoring and treatment
After the patient is transferred to the recovery room, intensive monitoring begins and, if necessary, treatment of complications is carried out. The latter are eliminated with antibiotics and special medications to maintain the operated organ. The tasks of this stage include:
- assessment of physiological parameters;
- eating as prescribed by the doctor;
- compliance with the motor regime;
- administration of drugs, infusion therapy;
- prevention of pulmonary complications;
- wound care, drainage collection;
- laboratory tests and blood tests.
Features of the postoperative period
Depending on which organs have undergone surgical intervention, the features of patient care in postoperative process:
- Organs abdominal cavity– monitoring the development of bronchopulmonary complications, parenteral nutrition, prevention of gastrointestinal paresis.
- Stomach, duodenum, small intestine - parenteral nutrition for the first two days, including 0.5 liters of liquid on the third day. Aspiration of gastric contents for the first 2 days, probing according to indications, removal of sutures on days 7-8, discharge on days 8-15.
- Gallbladder - special diet, drainage removal, allowed to sit for 15-20 days.
- Large intestine - the most gentle diet from the second day after surgery, there are no restrictions on fluid intake, the administration of Vaseline oil orally. Discharge – 12-20 days.
- Pancreas – preventing the development of acute pancreatitis, monitoring the level of amylase in the blood and urine.
- The organs of the thoracic cavity are the most severe traumatic operations, threatening blood flow disruption, hypoxia, and massive transfusions. For postoperative recovery, it is necessary to use blood products, active aspiration, and massage. chest.
- Heart – hourly diuresis, anticoagulant therapy, drainage of cavities.
- Lungs, bronchi, trachea – postoperative prevention of fistulas, antibacterial therapy, local drainage.
- Genitourinary system – postoperative drainage of urinary organs and tissues, correction of blood volume, acid-base balance, sparing caloric nutrition.
- Neurosurgical operations – restoration of brain functions and respiratory ability.
- Orthopedic and traumatological interventions - compensation of blood loss, immobilization of the damaged part of the body, given physical therapy.
- Vision – 10-12 hours of bed rest, walking from the next day, regular use of antibiotics after corneal transplant.
- In children - postoperative pain relief, elimination of blood loss, support of thermoregulation.

In elderly and senile patients
For a group of elderly patients, postoperative care in surgery has the following features:
- elevated position of the upper body in bed;
- early turning;
- postoperative breathing exercises;
- humidified oxygen for breathing;
- slow intravenous drip saline solutions and blood;
- careful subcutaneous infusions due to poor absorption of fluid in the tissues and to prevent pressure and necrosis of skin areas;
- postoperative dressings to control wound suppuration;
- prescription of a vitamin complex;
- skin care to avoid the formation of bedsores on the skin of the body and extremities.
Video
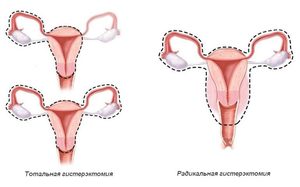
A hysterectomy is a surgical procedure in which the female reproductive organ is removed. This operation is very common in gynecology. The uterus is removed in cases where all other treatment methods have been ineffective. Sometimes the uterus is removed along with the fallopian tubes and ovaries. The postoperative period is an important stage in a woman’s treatment, which may be accompanied by the development of complications, so it requires a professional approach.
Surgery to remove the uterus is quite common, which is carried out for very serious illnesses that threaten a woman’s health. According to statistics, about a third of all women who have reached the age of 40 are forced to resort to such a procedure.
With any surgical intervention, injuries of varying severity occur, which are associated with damage to tissues and blood vessels. After a hysterectomy, damage also remains, and it takes time for the tissue to fully recover. The duration of postoperative rehabilitation depends on the severity of the disease, the type of surgery and postoperative complications.
More often removal of the uterus is indicated in the following cases X:
Depending on the severity of the disease carry out the following types of operations:
- removal of the uterus only;
- removal of the uterus and cervix (total extirpation);
- removal of the uterus with appendages and lymph nodes located nearby (radical panhysterectomy).
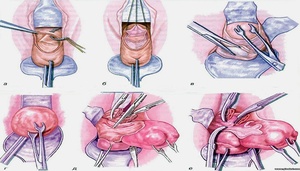
How severe the trauma will be depends not only on the type of operation, but also on the method of its implementation. The most radical is the abdominal technology, in which the walls of the peritoneum are cut, and another method is the vaginal method with an incision in the vagina. The least traumatic method is to remove the uterus using the laparoscopic method. In this case, a special laparoscope is used, which makes a very small incision. After laparoscopic surgery, complications are not so dangerous.
How long do you stay in hospital after a hysterectomy? It depends on the type of operation. After laparoscopy, the patient can be discharged the very next day. If abdominal surgery was performed, the patient can go home after 2 to 3 days.
Principles of rehabilitation
Recovery after surgery is divided into early and late stages. The early stage is carried out in a hospital setting under the supervision of a doctor. Its duration depends on the consequences that occurred after surgery. Early stage of recovery after abdominal surgery usually lasts 9–12 days, after which the doctor removes the stitches and the patient is discharged. After laparoscopy, early rehabilitation is reduced to 3.5 – 4 days.
 Main tasks early stage of rehabilitation are:
Main tasks early stage of rehabilitation are:
- relief from pain syndrome;
- elimination of bleeding;
- prevention of dysfunction of internal organs;
- avoiding infection of the affected area.
The late stage of rehabilitation is carried out at home. If complications do not develop after the operation, then recovery takes 28–32 days, and in case of complications it is extended to 42–46 days. This stage is characterized by complete tissue restoration, strengthening of the immune system, improvement general condition, normalization of the psychological state, complete restoration of performance.
What measures are taken immediately after surgery?
On the first day after surgery doctors take measures to eliminate painful symptoms, prevent complications and inflammatory processes from developing, eliminate blood loss from internal bleeding and prevent infection. This period is very important at the early stage of rehabilitation.
Key activities include specific activities.
Anesthesia. After the operation, the woman experiences natural pain in the inside and lower abdomen. To relieve pain, potent medications are prescribed.
Activation of organ functions. In this case, measures are taken to normalize blood circulation and stimulate the intestines. If such a need arises, then Proserpine is administered by injection to activate intestinal functions.
Diet. After surgery to remove the uterus and appendages, it is very important that normal intestinal motility is restored. The menu should consist of broths, drinks, pureed foods. If spontaneous defecation occurs at the end of the first day, it means that the event was carried out correctly.
Immediately after the operation the following drug therapy:
- antibiotics to prevent infection;
- anticoagulants to prevent the formation of blood clots in blood vessels;
- infusion effect carried out using intravenous droppers to restore blood volume and normalize blood circulation.
Complications during early rehabilitation
The first stage of rehabilitation may be accompanied by the following complications after hysterectomy:
How to recover after surgery? It is very important to prevent infection in the first 1–3 days. If this happens, the temperature rises to 38.5 degrees. To eliminate the risk of infection, the doctor prescribes antibiotics and carries out antiseptic treatment seam area.
Activities for late rehabilitation
After the woman is discharged from the hospital, her recovery from the hysterectomy continues. The late stage of rehabilitation allows the body to fully recover. Should the following actions are carried out:

It is very important to organize proper nutrition after removal of the uterus. A woman should not “push” and strain her abdominal muscles, so it is recommended to reduce the load on the intestines, trying not to eat aggressive and difficult-to-digest foods. The diet should be such that a laxative effect occurs.
Diet after hysterectomy includes the following approved products:
- crumbly porridge;
- green tea;
- vegetable oil;
- fresh vegetables and fruits (except grapes and pomegranates);
- mashed boiled vegetables;
- low-fat fermented milk products;
- boiled meat.
Diet after hysterectomy surgery prohibits the following dishes and products:
A diet after surgery should only be prescribed by a doctor.
Consequences
After extirpation of the uterus along with the ovaries, the location of many pelvic organs begins to change. This rearrangement negatively affects the health of the intestines and bladder.
Consequences after removal of the uterus for the intestines and bladder:
- constipation;
- the appearance of hemorrhoids;
- pain in the lower abdomen;
- difficulty going to the toilet;
- frequent urge to urinate without producing enough urine;
- urinary incontinence;
- problems with urine output that occur due to compression of the bladder.
 After surgery the patient may experience the development of vascular atherosclerosis, and a woman can also gain overweight. Lymphostasis of the extremities often develops during surgery. To prevent this from happening, the lymph nodes are removed during the removal of the uterus, ovaries and appendages. Amputation of the uterus and ovaries ends in premature menopause. The body begins to rebuild itself because a lack of estrogen leads to irreversible changes. Hot flashes appear very often.
After surgery the patient may experience the development of vascular atherosclerosis, and a woman can also gain overweight. Lymphostasis of the extremities often develops during surgery. To prevent this from happening, the lymph nodes are removed during the removal of the uterus, ovaries and appendages. Amputation of the uterus and ovaries ends in premature menopause. The body begins to rebuild itself because a lack of estrogen leads to irreversible changes. Hot flashes appear very often.
Thus, surgery to remove the uterus is quite traumatic surgical procedure. Recovery of the body after surgical treatment will be much easier and serious complications will not arise if all the doctor’s recommendations are strictly followed and healthy image life.
Attention, TODAY only!
DoctorVes.ru – website - 8-495-66-44-325
Day of the operation
You need to arrive at the clinic between 9:00 and 9:30 so that the nurse can prepare you for the operation. After completing your medical history, you will be taken to your room.
You need to take with you to the clinic:
- Passport
- The results of all tests, if you prepared them in advance (if some of the tests have not been done, they must be taken before 11 o’clock).
- A sheet that lists all medications (with doses), including nutritional supplements and vitamins that you take regularly.
- Pajamas or other comfortable light clothing.
- Toiletries (deodorant, soap, shampoo, razor and aftershave cream, etc.).
- Slippers.
- Hygienic lipstick.
- Lens container and solution (if you use contact lenses) Something to read (books, magazines, writing utensils) to keep you occupied after surgery.
- The clothes you will wear to go home after discharge.
- Women with preserved menstrual function must also take with them appropriate hygiene items (pads or tampons) regardless of the expected date of menstruation, since any operation, including bariatric surgery, is stressful for the body and can provoke a premature onset of menstruation.
- Please do not bring jewelry with you, as the clinic does not have a special safe for storing them.
A room (for example, a separate room for one person) will be selected for you according to your wishes if you inform us about this in advance.
If you have not called in advance, the availability of a private room upon your arrival cannot be guaranteed.
It is possible that all individual wards will be occupied at this time. Please note that your family and friends cannot stay with you if your room is a double room and there is a second patient in the room.
At the appointed time, you will be taken to the operating room, where immediate preparation for the operation begins (an intravenous catheter will be installed in the vein of the forearm or subclavian vein for administering medications during and after the operation). Doctors, nurses, and anesthesiologist will ask you several questions. The anesthesiologist will give you a sedative (intravenously) to keep you calm and relaxed. The operation is performed under general anesthesia. The patient does not feel anything and wakes up in the room.
Your relatives and friends can accompany you to the entrance to the operating room, but they are not allowed to enter the operating room itself - they can wait for the end of the operation in the department.
Depending on the type of operation, it can last from 30 minutes (gastric banding) to 3-4 hours (other operations), although sometimes, in particularly difficult cases, the duration of the operation can reach 5-6 hours. Family members are not allowed in the recovery and intensive care room, where you may be admitted for several hours after surgery.
After the operation, you will be taken to a ward or to the intensive care unit for several hours, where you will remain until your condition stabilizes and normal breathing and consciousness are restored.
On the evening of the day of surgery
Painful sensations.
Pain during the first days after surgery is usually mild and can be easily relieved by taking painkillers. Moreover, some patients require pain relief altogether.
Motor activity.
It is very important to get up at least once in the evening after surgery. When you get up for the first time, this must be done with the help of clinic staff, relatives or roommates, as you may feel dizzy. First you need to sit for about 5 minutes; If you don’t feel dizzy after this, you can get up. If there are no problems with being in an upright position, you can walk without restrictions, focusing on your well-being. This active regimen prevents the formation of blood clots in the veins of the legs and prevents the development of congestive pneumonia (pneumonia).
Please do not leave without first informing the nurse that you want to get up and walk, you are strongly discouraged from walking unaccompanied. In particular, painkillers can affect the coordination of your movements.
Compression stockings (or their equivalent - elastic bandages) must be worn before surgery and then, during the postoperative period, stockings or bandages should be worn as prescribed by the doctor. Compression stockings will help prevent the formation of blood clots and their migration from the venous system lower limbs. It is possible that additionally
You will receive anti-clotting medications (eg heparin, subcutaneously), which also helps prevent thrombosis (blood clots forming and spreading through the blood vessels). Compression stockings and bandages do not need to be worn during gastric band surgery, provided there are no blood clotting problems.
Is it possible to eat and drink?
If you have had gastric bypass, sleeve gastrectomy, or MAG, you should not consume food or water. You can moisten and rinse your mouth without swallowing the liquid.
After gastric band surgery, after 4-5 hours you can drink a small amount of water (periodically 1-2 sips), mainly to wet the mouth. If water passes into the stomach freely, you can have a light breakfast the morning after surgery.
Breathing exercises
It is very important to take deep breaths and exhale 10 times within an hour. If you want to clear your throat, you can and should do so. A simple breathing exercise of inflating is very helpful. rubber toys, balls Or balloons (useful to have with you). They need to be done several times every hour. Such breathing exercises are needed to avoid congestive pneumonia (pneumonia).
If you have any problems with respiratory system For example, if you suffer from bronchial asthma or chronic bronchitis, please bring the inhalers you use with you and follow the course of inhalations prescribed to you previously (before surgery).
Bladder function
Usually in the evening after surgery the patient gets up and goes to the toilet on his own. If you have any problems urinating on your own, tell the charge nurse. If in the process of preparing for surgery it becomes necessary to install a urinary catheter, it must be removed before standing.
Nausea and vomiting
Nausea and vomiting after surgery should be avoided. If you experience nausea, do not wait until vomiting appears, tell the medical staff. You will be prescribed medications.
Leg exercises
In order to prevent blood stagnation in your legs and blood clots from forming, on the first day after surgery, you need to do simple exercises for the legs, which consist of maximum flexion and then maximum extension of the foot.
The day after surgery
The next day after surgery, you need to not only get out of bed, but start actively walking around the department. Such physical activity has a positive effect on all body functions.
If the patient has undergone gastric banding, you can drink without restrictions, and intravenous administration(drip) can be stopped. If an IV is not prescribed, you need to drink at least 2 liters of liquid per day. You can drink any liquids without sugar and without gas, for example:
- Plain water
- Not strong (not hot) tea
- Not strong warm coffee
- Mineral water
If desired, you can add sugar or its substitutes. If you want to eat, then the optimal food may be food in the form of yogurt, banana, pureed soups, purees.
As a rule, after making sure that water passes easily into the stomach and the pain in the area of surgical punctures is tolerable, we discharge patients who had undergone gastric band surgery the day before the next morning. The dressing is done, the stickers are changed, and the catheter is removed from the vein. After this, the patient is sent home.
After gastric bypass (as well as sleeve gastrectomy and MAG), testing of the upper gastrointestinal tract is usually done before the patient is allowed to drink and eat. You will be given a special X-ray contrast agent to drink, then the X-ray room will determine the passage of this substance through the esophagus, stomach and intestines. After this, you will be allowed to drink 1 liter of fluid per day. You should not eat food the day after such operations. The day after bypass surgery or gastroplasty, the patient is prescribed intravenous fluids (drip).