In the emergency department complaints Patients with pain in the shoulder area can be heard quite often. This amazing joint has a very wide, almost full range of motion. The extensive ligamentous and muscular apparatus makes it a complex joint, as a result of which differential diagnosis between individual nosological units can be difficult. The tendons are adjacent to the articular capsule, fused with it in places.
Muscles, tendons and ligaments provide stability and hold the humerus in correct position in the glenoid cavity of the scapula, counteracting the force of gravity. Gravity tends to disrupt stability shoulder joint, pulling the humerus down from the socket. Head humerus has very weak contact with the hollow glenoid cavity of the scapula.
Shoulder girdle actually consists of three joints: sternoclavicular, acromioclavicular and glenohumeral and one connection - the scapula with chest. These joints have a very complex relationship with the movements of the shoulder, and it is in them that pathological processes most often develop, manifested by pain in the shoulder joint. The figure shows the normal anatomy of bones and ligaments, which should be well known in order to be able to understand diseases in the shoulder area.
Higher bundles shown in the figure, there are muscles that support the humerus and give it the ability to perform a full range of movements.
Shoulder joint surrounded by the rotator cuff, consisting of the teres minor, infraspinatus and supraspinatus muscles, attached to the greater tuberosity, and the subscapularis muscle, attached to the lesser tuberosity. Superficial to these muscles is the deltoid, the action of which is to raise the head of the humerus, moving it under the coracoacromial arch and abducting the shoulder.
Arm-torso mechanism. The glenohumeral joint and scapulocostal synchondrosis act as a single unit when the shoulder is abducted. The ratio of movements of the scapula to the glenohumeral joint is 1:2, therefore, for every 30° of abduction of the arm, the scapula moves 10° and the glenohumeral joint moves 20°. With a completely immobilized glenohumeral joint, scapulothorbital synchondrosis is capable of providing abduction of the arm by 65°. This is called the "shrug" mechanism. For the emergency physician, knowledge of this mechanism is important for assessing movement in the shoulder joint affected by any pathological process.
IN sternoclavicular joint During the first 90° of abduction, the clavicle rises 4° for every 10° of shoulder abduction. When abducted more than 90°, movement in this joint disappears. The range of motion in the acrominoclavicular joint is approximately 20°. These movements occur during the first 30° and after 100° of abduction. When the upper limb is adducted, the clavicle rotates along its long axis.
 Ligaments of the shoulder joint. SDM - biceps tendon; N PS - inferior glenohumeral ligament; MHL - middle glenohumeral ligament; SHL - superior glenohumeral ligament; CAD - coracoacromial arch; ACL - acromioclavicular ligament; TC - trapezoid ligament; CL - conical ligament; SCL - sternoclavicular ligament; RCL - costoclavicular ligament
Ligaments of the shoulder joint. SDM - biceps tendon; N PS - inferior glenohumeral ligament; MHL - middle glenohumeral ligament; SHL - superior glenohumeral ligament; CAD - coracoacromial arch; ACL - acromioclavicular ligament; TC - trapezoid ligament; CL - conical ligament; SCL - sternoclavicular ligament; RCL - costoclavicular ligament
Basic anatomy of the shoulder joint and acromioclavicular joint
In the area shoulder joint you can easily palpate a number of structures that the emergency physician should know well, since they are typical sites of localization of pathological processes.
If palpate The supraclavicular notch, moving outward, can identify the sternoclavicular joint. The clavicle is located just above the manubrium of the sternum and at this point its proximal end can be easily determined. The clavicle is located subcutaneously along its entire length and is easy to palpate. In the outer third, the clavicle begins to flatten, but at the very end, protruding above the acromion process, it again takes on a rounded shape.
 The ratio of the range of motion in the glenohumeral joint and the scapulocostal joint
The ratio of the range of motion in the glenohumeral joint and the scapulocostal joint
AC joint palpated just medial to the distal end of the clavicle, protruding above the flattened acromion process. It is easier to identify the acromioclavicular joint if, during palpation, you ask the patient to move the shoulder several times. The greater tubercle of the humerus is located lateral to the acromion process and can be easily felt if you follow the acromion process to its outer end and then slide your fingers down. There is a small step between the outer edge of the acromion process and the greater tuberosity.
Biceps tendon groove(intertubercular groove) is located anterior and medial to the greater tubercle and is bounded laterally by the greater tubercle and medially by the lesser tubercle. This structure is easier to palpate if the hand is rotated outward. With external rotation, the groove moves to a place more convenient for palpation, which allows the doctor to first palpate the greater tubercle, then the intertubercular groove and, finally, moving in the medial direction, the lesser tubercle.
 The most important synovial bursae of the shoulder joint
The most important synovial bursae of the shoulder joint
Inside this furrows lies the biceps tendon. The coracoid process can be palpated by asking the patient to relax and noting the deepest part of the concavity of the clavicle, which is located on the outer third. The fingers are then placed approximately 2.5 cm below the anterior edge of the collarbone. By pressing with your fingers in an outer and posterior direction, you can feel the coracoid process. The coracoid process can also be detected by palpation of the deltoid-thoracic triangle. The scapula can be viewed from behind; it covers the space from the 2nd to 7th ribs.
Rotator cuff, although it is not easy to palpate, it must be examined, since it is a common site of occurrence of pathological processes. Its localization and location are shown in Fig. 276. In the area of the shoulder joint there are four synovial bursae. The most important of them is the subacromial, or subdeltoid, located between the deltoid muscle and the rotator cuff and extending under the acromial process and the coracoacromial arch, separating these structures from the muscles that form the rotator cuff.
Subcoracoid bursa localized under the coracoid process. The subscapularis bursa is located near the tendon junction of the subscapularis muscle with the lesser tubercle. The scapular bursae are located at the upper and lower inner edges of the scapula and are separated from the chest wall.
Diseases shoulder joint area It is advisable to divide into three groups: diseases of the shoulder joint; diseases of the muscles, tendons and bursae of the shoulder joint and, finally, diseases of scapular-costal synchondrosis.
Acromioclavicular joint - articulation shoulder girdle upper limb, formed by the collarbone and scapula. This element of the musculoskeletal system, due to its anatomy, does not perform a large range of movements, but has great clinical significance due to the development of pathological processes in it.
Anatomy
The formation of the articulation involves two articular surfaces of the bones of the upper limb girdle: the clavicle (its humeral end) and the scapula (the process of the acromion). The bone structures are supplemented with a cartilaginous element - the articular disc of the acromioclavicular joint.
It divides the capsule into two cavities, participates in feeding the elements and cushioning movements.
Movements
The articular surfaces lie relative to each other in such a way that movements along several axes in a large volume are possible in the articulation. However, thanks to the powerful ligamentous apparatus, mobility is physiologically reduced and movements in the joint are minimal.
This arrangement of the anatomy of the joint allows the joint to perform a supporting function and hold the movable upper limb in the shoulder girdle.
Joint ligaments
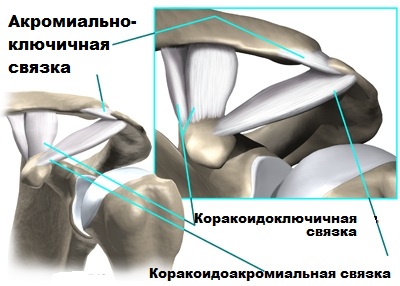
Along the edges of bony articular surfaces lined with hyaline cartilage tissue, the fibers of the joint capsule are attached. The following formations give additional strength to the shell:
- Acromioclavicular ligament. It fixes the humeral end of the clavicle and the acromion of the scapula together.
- Coracoclavicular ligament. This structure serves as an additional fixing element - it holds the coracoid process of the scapula at the humeral end of the clavicle.
Between the ligamentous elements there is a space in which the fiber is located. This adipose tissue is an additional shock absorber; in addition, blood vessels feeding the surrounding tissues pass through it.
Ligaments of the scapula

The scapula is a flat bone, has insufficient bone strength, but bears a large load due to two joints. Therefore, there are ligaments that complement its function and strengthen elements. These include:
- Coracoacromial ligament. It runs from one process of the scapula to the other. It contains very strong fibers and reliably holds the coracoid and acromial processes together.
- Superior transverse scapular ligament. Thanks to this element, the notch of the bone tissue of the scapula at its upper end forms an opening through which the functionally important suprascapular nerve passes.
- Inferior transverse ligament. A small structure stretched between the acromion and the capsule of the shoulder joint. Plays the least role in fixing the joint.
Pathology of the joint
This anatomy is aimed at performing the main function - support, which can be disrupted under the influence of damaging factors. Diseases of the acromioclavicular joint include:
- Dislocations and...
- Arthrosis of the acromioclavicular joint.
Inflammatory pathology (arthritis) rarely develops, since the joint is surrounded by soft tissue and it is not easy for an infectious agent to penetrate inside the capsule.
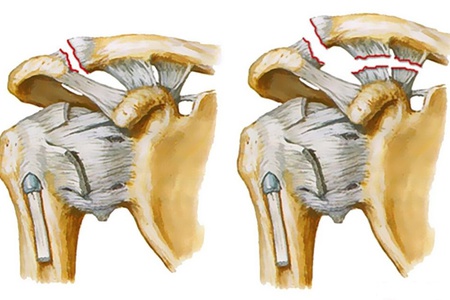
Articulation tears
This disease is a very common pathology both during heavy sports loads and in everyday life due to falls and injuries. Rupture and dislocation of the joint are synonymous in the case of the acromioclavicular joint, since displacement of the articular surfaces (a necessary component of dislocation) is impossible without violating the integrity of the ligaments that hold the elements together.
Reasons
What can lead to rupture of strong ligamentous elements scapular region? The most common cause of injury is a fall on the shoulder area. Body weight, exceeding the shock-absorbing capacity of the ligaments, acts on the tendons of the scapula. The fibers cannot withstand the load and break.
The likelihood of falling increases when playing game sports, skiing, and also in the winter season, when falls are caused by slipping on ice.
Symptoms and diagnosis

Manifestations of the disease will depend on the degree of ligament rupture. The following types of damage are distinguished:
- Stretching. At initial stage there is pain in the projection of the joint, increased mobility due to sprain of the joint ligaments. There is no violation of the integrity of the ligaments.
- Rupture of one of the three fibrous structures (most often the acromioclavicular ligament). The damage is accompanied by the development of edema and hematoma. Movements are sharply painful and sometimes impossible.
- Complete rupture of ligaments and dislocation of the joint. In the third degree, there is an accumulation of blood in the joint cavity, intense pain, and severe instability in the joint. Swelling grows above the capsule, visually identified as a lump. When trying to move, a crunching sound is heard in the projection of the capsule, and the pain increases sharply.
The diagnosis is made on the basis of anamnesis, clinical picture disease, physical examination data. The doctor will order an x-ray of the shoulder girdle to rule out a fracture. MRI (magnetic resonance imaging) will help make a definitive diagnosis thanks to visualization of the ligaments, but due to the high cost of the procedure, it is most often abandoned.
Treatment
The choice of treatment method will depend on the severity of the injury. For first and second degree ruptures, the shoulder is immobilized (immobilized) using modern bandage devices or a bandage. To relieve pain, non-steroidal anti-inflammatory drugs (nimesulide, diclofenac, ibuprofen) are prescribed.
The third degree of rupture, accompanied by dislocation of the joint, can also be treated conservatively, but with this method there is a high risk of developing arthrosis of the acromioclavicular joint. Therefore, it is advisable to resort to surgical intervention.
Under general anesthesia, through an incision above the joint capsule, the articular ends of the bones involved in the formation of the joint are compared. To hold them in the desired position, you may need fixators (screws) or a tendon suture.
After the intervention, immobilization of the limb is also prescribed.
Arthrosis of the acromioclavicular joint

Under the influence of traumatic factors, frequent loads on the shoulder girdle, and improper treatment of damage to the joint, a pathology such as arthrosis (osteoarthritis) of the acromioclavicular joint can develop.
The disease is characterized by detachment of cartilage tissue from bone surfaces, degeneration of joint tissue, and the proliferation of spinous projections. All of these factors disrupt the comparability of the articulation elements, movements become painful, and local inflammation develops.
Symptoms
Manifestations of the disease depend on the duration of the disease, associated factors, general condition body. When the first degenerative changes appear, the patient notices pain when moving the joint, which also occurs when palpating the joint.
As the degree of degeneration increases, the pain intensifies; it always increases in the evening, after intense exercise or heavy lifting. There is a crunching sensation and a feeling of instability in the joint.
In the late period of the disease, the listed symptoms are accompanied by limitation of mobility up to contracture. Crossing your arms over your chest becomes impossible due to pain and degeneration of the joint. With this degree of disease, treatment is only surgical.
Diagnostics

When carrying out diagnostic measures, the doctor will definitely ask the patient about past injuries, sports, and heavy physical labor. To establish a diagnosis in the later stages, anamnesis and clinical examination of the patient are sufficient.
Supporting studies are:
- X-ray of the shoulder girdle.
- Magnetic resonance imaging.
- Ultrasound of the acromioclavicular joint.
All methods, to one degree or another, can indicate signs of degeneration of articular surfaces, the presence of osteophytes (outgrowths of bone tissue), and the condition of the collarbone and scapula.
Another valuable diagnostic method is puncture. During this procedure, a certain amount of joint fluid is drawn into a syringe, which is then subjected to microscopic examination. The analysis will indicate the presence of signs of inflammation, the presence of microorganisms in the cavity of the joint capsule, and rheumatoid factor - a marker of rheumatic diseases.
Treatment
Treatment of arthrosis, a severe degenerative disease, often requires the use of several treatment methods at once. Only an integrated approach can effectively relieve symptoms and lead to regression of the disease. The following are used in therapy:
- Drug treatment.
- Physiotherapy.
- Massage and exercise therapy.
- Surgical intervention.
Drug treatment

From medicines nonsteroidal anti-inflammatory drugs, hormonal medications, and muscle relaxants are used. The first group of drugs is necessary to reduce the intensity of the inflammatory syndrome. Tablets, intramuscular and intravenous injections, gels and ointments with NSAIDs eliminate pain, swelling, and improve joint mobility.
Hormonal drugs (diprospan) are injected into the joint cavity and effectively reduce pain, but frequent use of such drugs is not recommended.
Muscle relaxants are used in the later stages of the disease, when long-term inflammation leads to reflex muscle spasm of the shoulder girdle. A drug such as mydocalm can relax muscles. Its use quickly leads to symptomatic relief.
Physiotherapy
To enhance the effect medicines The use of physiotherapy methods is recommended. These procedures alleviate symptoms, eliminate inflammation, and have a positive effect on the prognosis. These include:
- Electrophoresis.
- Electromyostimulation.
- Ultrasound.
- Magnetotherapy.
All methods have their own contraindications, so they are prescribed by the attending physician.
Massage and exercise therapy
![]()
Therapeutic exercises effectively influence the prognosis of the disease both during isolated conservative therapy and after surgery on the joint. Exercises are performed gradually, after the recommendations of the attending physician.
Surgical intervention
Surgery is necessary for arthrosis of the acromioclavicular joint, if the disease has reached severe irreversible stages. Plastic surgery is performed through a classic incision or by arthroscopy (using a camera and micro-instruments).
The acromioclavicular joint can restore its function and physiological anatomy only if the patient follows the doctor’s recommendations.
How to forget about joint pain?
- Joint pain limits your movements and full life...
- You are worried about discomfort, crunching and systematic pain...
- You may have tried a bunch of medications, creams and ointments...
- But judging by the fact that you are reading these lines, they did not help you much...
But orthopedist Sergei Bubnovsky claims that indeed effective remedy for joint pain exists!
This disease is a natural aging process, the physiological wear and tear of human joints. The disease is inflammatory in nature, which is accompanied by a dystrophic-degenerative effect. If the disease is detected at the first stage of development, it can be quickly and easily cured. However, advanced arthrosis is not so easy to overcome; more effort and an integrated approach to the problem will be required. Often, clavicular acromial arthrosis is accompanied by pain in the shoulder area; a little less often, pain is felt in the legs.
Causes of arthrosis
Acromioclavicular arthrosis usually occurs due to the body's natural aging processes, which begin in people over 40 years of age. Often the disease is diagnosed in a patient who has suffered a bad fall or suffered a serious injury or bruise. Another cause of arthrosis may be a dislocation of the shoulder, which occurred to a person several years ago. A sign of clavicular acromial arthrosis is pain in the shoulder joint, which causes difficulties in performing usual household work.
Stages and symptoms of the disease
- Clavicular acromial arthrosis of the 1st degree does not express clear symptoms, so the disease is rarely diagnosed at the initial stage of development. The first stage is characterized by mild pain when pressed in the area of the collarbones or during certain movements of the arms and shoulder joints. Rarely, pain is also felt in the spine and neck. For this reason, the disease progresses slowly.
- Arthrosis of the acromial clavicular joint of the 2nd degree is accompanied by aching pain in the shoulder, which leads to difficulties when changing clothes, crossing your arms over your chest, placing them behind your head or back. If the cause of clavicular acromial arthrosis is injury, the shoulder joints may produce a characteristic crunching or clicking sound.
- Grade 3 clavicular acromial arthrosis is characterized by constant pain and bone deformation. Moreover, the affected joint becomes completely immobilized. When palpating the area where the shoulder joins the scapula, bone growths and protrusions are felt. The last stage of arthrosis is rare, since diagnosis and treatment of pathology begins more often at the second stage of development of the disease.
Symptoms of clavicular acromial arthrosis are:
- fatigue;
- pain in the shoulder and collarbone area;
- stiffness of movement of the shoulder joint;
- clicking or crunching in the shoulder.
Diagnostic methods
The sooner the patient consults a doctor, the easier the treatment of the disease will be. Primary diagnosis involves interviewing and examining the patient by the attending physician. You must answer questions about when the symptoms began, whether you have had injuries to your limbs, shoulders, or collarbone, what shoulder and arm exercises are difficult for you to do, and in what specific area the pain occurs.
To confirm the diagnosis, a so-called “diagnostic blockade” is required, the essence of which is the doctor injecting a small amount of an antisthetic (Lidocaine is often used) into the cavity of the clavicular joint. If a rheumatologist has discovered an inflammatory process in the clavicular joint in a patient, then after the injection the pain immediately goes away. To complete the picture of the disease, the doctor, as a rule, refers for an X-ray examination, after which he prescribes complex surgical treatment.
Treatment of acromioclavicular arthrosis
Like many other diseases, arthrosis of the acromioclavicular joint requires complex treatment. It can be either aggressive or mild, depending on the degree of the disease. At the first stage of arthrosis development, patients often do without non-steroidal anti-inflammatory drugs or other potent drugs to relieve symptoms. Doctors prescribe long courses of chondroprotectors for patients with any stage of acromioclavicular arthrosis. The drugs gradually restore the damaged articular cartilage.
Doctors turn to aggressive therapy for arthrosis at the second or third stage of the patient’s disease. To relieve severe pain, the doctor may prescribe active painkillers. This approach does not relieve the patient of clavicular acromial arthrosis, but effectively copes with its symptoms. An alternative to this treatment is traditional methods, which help to activate blood circulation, increase the body’s immunity and saturate it with useful elements.
Drug treatment

Conservative treatment of clavicular acromial arthrosis involves providing the patient with rest and prescribing anti-inflammatory drugs, for example, Ibuprofen, Aspirin, Diclofenac, Voltaren. Such remedies relieve the patient from severe pain and relieve swelling from the affected joint. Glucocorticosteroids such as Kenalog or Diprospan perform a similar function. If the above medications do not help, your doctor may prescribe a Cortisone injection into the joint. This remedy is considered one of the strongest painkillers, but its effect is temporary.
To restore damaged cartilage, patients take chondroprotectors, which include Chondroitin-AKOS, Teraflex, Chondrolone, Artra and others. These products contain substances that are produced by a healthy body themselves; they are needed for the formation of synovial fluid. If a patient with clavicular acromial arthrosis is bothered by spasms, the doctor prescribes muscle relaxants (Mydocalm, Baclofen).
Physiotherapeutic methods
- Application of sinusoidal modulated currents
This type of treatment for clavicular acromial arthrosis is applicable only in cases where there is no inflammation of the joint and there is pain. As a rule, doctors prescribe modulated currents to elderly patients with advanced disease that is difficult to treat. Contraindications are heart disease (bradycardia, arrhythmia).
- Ultrahigh frequency therapy

The effect of the method is to change the charge of tissue cells through a displacement current. Due to this, tissue conductivity improves, which facilitates access to the affected area of various medications that the patient is taking. Ultrahigh-frequency therapy restores the normal permeability of the cells of the inner lining of blood vessels, thereby stopping the excessive release of plasma outside the vessels. This has a positive effect on the process of reduction of joint swelling.
- Infrared irradiation
The length of the infrared waves will differ, depending on the degree of the disease and the doctor’s special instructions: from a few centimeters to decimeters. Long waves are used more often. Their penetration into the affected tissues is deeper, so the effect of such waves on arthrosis deformans is more effective. The advantage of this treatment method is the absence side effects and contraindications.
- Acupuncture
The principle of acupuncture is the external influence on specific points that are associated with certain human organs. Through acupuncture, a nerve impulse is transmitted to a specific organ or area of the body, stimulating changes in that area. Using this treatment method, the doctor can increase the tone of the patient’s muscles and blood vessels, activate blood flow in a joint or limb affected by arthrosis, and normalize metabolic processes.
- Hirudotherapy
The effectiveness of this method for clavicular acromial arthrosis is explained by the fact that thanks to leeches, blood circulation improves and lymphatic congestion is eliminated. By sucking, this annelid injects biologically active substances into the patient’s vessels - bdellins, hirudins, elgins and others. These enzymes dissolve blood clots, normalize metabolism, increase immunity and elasticity of tissues in the human body.
- Apitherapy
The method is based on the use of bee venom in the treatment of clavicular acromial arthrosis. Apiprugs and apitoxin, which are contained in bee venom, when entering the patient’s body, affect the prostaglandins contained in his body. Thanks to this, pain sensitivity is reduced in case of deforming clavicular acromial arthrosis.
- Massage

The effectiveness of massage lies in a significant reduction in pain in patients with clavicular acromial arthrosis. With the help of therapeutic massage, lymph circulation of damaged joints is improved, tissue supply is activated nutrients and oxygen, prevents the development of limb stiffness or muscle atrophy.
In order to quickly restore damaged joints, the doctor prescribes physical therapy (physical therapy) classes. First of all, he draws up a special exercise program that in the best possible way suitable for the patient, taking into account his individual characteristics. The course of therapeutic exercises lasts from 1 month to six months. After visiting a trainer, you need to continue exercising at home.
Surgical intervention
If an orthopedist diagnoses a third-degree acromioclavicular arthrosis in a patient, the patient will undergo surgery, since other treatment at this stage is no longer effective. Often modern medicine resorts to endoprosthetics or arthroplasty of the shoulder joint. Arthroplasty surgery involves removing the acromial end of the clavicle. Scar tissue then fills the gap between the acromion and the collarbone, forming a false articulation.
As a result of this procedure, the connected parts do not experience much stress. Arthroplasty is usually done through a small incision in the skin directly over the diseased joint. Some modern doctors perform the operation using an arthroscope - an instrument with a mini video camera at the end, which allows the surgeon to work with greater precision.
Folk remedies
- Treatment of arthrosis with horseradish root compresses. Grind the horseradish root with a grater, wrap the shavings in gauze and place in a container of water, wait until it boils and cool. Wrap the pulp in a canvas cloth moistened with water in which the horseradish was boiled, and place it on the areas affected by arthrosis. Leave the compress on for 30-60 minutes, doing it daily for 14 days. This folk remedy will relieve swelling and activate blood flow to the joint damaged by arthrosis.
- Treatment of arthrosis with iodine lotions. Mix 5% medical iodine, flower honey, ammonia, glycerin, and medical bile in equal proportions. Infuse the product for 10 days in a dark, cool place. Before use, shake the mixture, pour some into a small jar and heat in a water bath. Moisten a napkin with the prepared solution and place it on the joint affected by clavicular acromial arthrosis, leaving it overnight. Place cellophane on top and tie with a bandage. Repeat the procedure daily until recovery.
- Treatment of arthrosis with cabbage compresses. Take a medium head of cabbage, cut it into small pieces and mash them with your hands. Pass the resulting mass through a juicer or meat grinder. Soak a piece of woolen cloth in cabbage juice until it is completely saturated, and apply it to the joint with arthrosis. Repeat the procedure every evening for a month. The finished juice is suitable for use for no more than 3 days.
Rehabilitation period
After the operation, the patient's arm is immobilized for 14 days using a bandage. For 6 weeks, a patient with arthrosis should limit physical activity, and after this time has elapsed, the shoulder is allowed to be loaded in full. During rehabilitation, the patient is prescribed a complex physical therapy, massage, cryotherapy. First, exercises are performed to increase the range of motion of the joint. After a certain time, the patient needs to focus on strengthening the muscles, gradually increasing the load to prevent relapse.
Disease prevention
Like any other activity, fitness helps reduce a person’s weight, activates blood circulation, strengthens muscles - this is extremely important for the prevention of arthrosis. However, moderation is important. Excessive load on the joints and incorrect exercise technique can, on the contrary, lead to further big problems. Therefore, it is better for a patient with clavicular acromial arthrosis to first practice under the supervision of a doctor. Exercises in the pool have an excellent effect; you can do them in addition to the main load.
Except physical exercise, a patient with clavicular acromial arthrosis should change his diet. To prevent the disease, it is better to refrain from eating fatty foods, including red meat. In return, supplement the menu with seafood and fish, fresh fruits, and vegetables. Gelatin and cartilage will be beneficial for joints. Doctors recommend that patients increase the amount of water consumed to 3 liters per day. You can take a course of vitamins B, A, D and calcium. Prevention of clavicular acromial arthrosis will include:
- wearing orthopedic shoes;
- getting rid of excess weight;
- protection of joints from cold;
- healthy eating, correct sleep mode.
Video: how to defeat arthrosis of the acromioclavicular joint
Patients over forty years of age often develop clavicular acromial arthrosis. This disease initially occurs without symptoms, without causing obvious discomfort or pain to the person. However, in certain cases, severe pain is observed in the area above the affected joint. They gradually intensify, which is especially felt when moving the shoulders. Treatment of clavicular acromial arthrosis is performed in a complex manner. The video explains how to cure this disease.
“Like no hands” - who doesn’t know this expression! Indeed, the lack of the possibility of normal, full movement of the arms puts a person in a limited position. The upper limbs and shoulder girdle are quite complex, and it is quite easy to damage them, especially the ligamentous apparatus. A good example is the acromioclavicular joint, where diseases or injuries are widespread.
Joint structure
A joint is formed when two bones join: the acromion process of the scapula and the end of the clavicle, located next to the shoulder joint.
Bone formations
The clavicle is a small tubular bone of the shoulder girdle. On one side it connects to the sternum, forming the sterno-clavicular joint. The second end attaches to the acromial process of the scapula - this formation is called the acromioclavicular joint.
The sternum is a supporting bone with a spongy structure. It has no mobility, so the health of the joint connecting it to the collarbone is important. This articulation allows upper limbs make upward movements, put your hands behind your head, rotate them around your axis. It is this wide range of possibilities that allows you to carry out daily life activities.
Also, a healthy joint between the collarbone and sternum makes it possible to:
- exercise;
- master professions related to active hand movements.
Diseases or injuries of this joint of various origins lead to disruption of the usual way of life or the inability to engage in professional activities.
The humeral end of the clavicular bone connects to the scapula at the acromioclavicular joint. This is a flat bone that has no supporting function, but carries the most important load associated with the connection of the bones of the shoulder girdle. It must ensure the strength and activity of two joints: the shoulder and clavicular.
The movements of this anatomical formation are in mutual planes, so the bones are connected to each other not only by bone surfaces and muscle formations, but there is a very complex ligamentous apparatus.
Ligament device
Movement in this joint requires special strength and elasticity, which is provided by a complex ligamentous apparatus:
- acromioclavicular;
- coracoid - clavicular.
 They are complemented by the ligamentous structures of the scapula: coracoacromial, superior and inferior transverse ligaments. Each of them carries out the necessary functions. They are additional formations for the connection with the collarbone, which provide nutrition, strength, elasticity of the connection, and protect the nervous and vascular elements from injury during movement.
They are complemented by the ligamentous structures of the scapula: coracoacromial, superior and inferior transverse ligaments. Each of them carries out the necessary functions. They are additional formations for the connection with the collarbone, which provide nutrition, strength, elasticity of the connection, and protect the nervous and vascular elements from injury during movement.
The acromioclavicular ligament elastically connects the clavicle bone to the corresponding process of the scapula. The coracoclavicular ligament provides an additional connection and holds the scapula directly to the collarbone.
Cartilaginous structures
The articular surfaces of both bone structures are covered with cartilage tissue and are separated by an articular disc. Thus, the internal cavity of the acromioclavicular joint is divided into two chambers. The functions of this cartilaginous disc are as follows:
- mitigation of shock effects of movements;
- congruence of connected elements;
- division of the joint capsule into two cavities.
Each of the above points is necessary to ensure full range of motion.
Motion absorption
This means mitigating the impact of walking, hitting, and rotating movements. If there were no disc formation, then the surfaces of the acromion (the process of the scapula) and the clavicular bone would hit each other with any movement, which would inevitably lead to early destruction of the joint. Actually, this is what happens with regular or professional injuries to the joint in question.
Congruence of articular elements
This concept means the complete correspondence of mutually adjacent surfaces to each other. However, the surfaces of the bones may not always completely coincide at the articular surfaces.
It is this function that is performed by the articular disc, which provides the acromioclavicular joint with complete coincidence of the corresponding surfaces, which ensures the physiological volume of motor reactions.
Separation of the joint capsule
The need to divide the articular internal capsule into two isolated chambers has developed and been consolidated in the course of evolution. This structure ensures movement in different planes:
- vertical;
- horizontal;
- rotational movements.
Without such a formation as the articular disc, such movements would be impossible.
Causes of pathology
Problems with fullness or pain in movements of a given joint can occur for various reasons:
- age-related changes;
- injuries;
- metabolic diseases;
- occupational diseases.
Age-related changes
With age, especially after forty years, the elasticity of ligamentous structures is lost. Blood supply and nutrition of the constituent elements deteriorate.
There may be a limitation in the range of movements due to pain when performing them.
Injuries
In the course of life, almost every person receives injuries to one or another joint.
 This articulation is subjected, perhaps, to the most wide range similar influences. Dislocations, ruptures, sprains, and tears of ligaments occur here. The cause of such traumatic effects can be:
This articulation is subjected, perhaps, to the most wide range similar influences. Dislocations, ruptures, sprains, and tears of ligaments occur here. The cause of such traumatic effects can be:
- playing sports;
- domestic injuries;
- occupational diseases.
Athletes often perform heavy exercises aimed at training the shoulder girdle. The quantity and intensity of training, especially big sports, lead to wear and inflammation of the ligamentous apparatus. Elastic formations cannot withstand such loads, so athletes often suffer from ruptures and sprains of the ligaments.
Getting a clavicular joint injury in everyday life is not difficult. A sprain is manifested by pain, swelling and redness of the surface above the joint may occur. The first sign is pain, a sharp limitation of joint movements.
Occupational diseases
In occupational diseases, symptoms develop gradually. First, there is a slight soreness in the projection of the joint. Then the appearance of a persistent pain reaction when performing a small range of movements.
 The next stage is characterized by constant pain without external stimuli. Joint deformation, inability to move, and pain at rest may occur.
The next stage is characterized by constant pain without external stimuli. Joint deformation, inability to move, and pain at rest may occur.
Professions such as painter-plasterer, loader, performing monotonous movements on a conveyor belt, and construction professions are the most risky in terms of developing pathology of the joints of the upper shoulder girdle.
Every person has a risk of developing pathology of the scapuloclavicular joint. Age-related changes and injuries eventually lead to problems with nutrition and elasticity of the articulation elements.
If symptoms of pain, restriction of movement, or swelling appear, you should immediately consult a doctor for advice; self-medication can lead to disastrous consequences.
Preventing Shoulder Injuries provides a warm-up before starting sports activities, developing flexibility and strength in the pre-season period and maintaining them throughout the entire competition season, correct technique and appropriate equipment, as well as knowledge of injuries common to the sport.
To understand the essence shoulder complex injuries, you need to know its anatomy and biomechanics. The shoulder or glenohumeral joint has a spherical shape and is formed by the head of the humerus and the glenoid cavity of the scapula. The shoulder joint is anatomically and biomechanically closely related to the scapula and collarbone and forms with them the so-called shoulder girdle.
Top of the shoulder joint covered by the coracoid process of the scapula, acromial and coracoacromial ligaments. The shoulder joint is a four-freedom joint. The shoulder joint is surrounded by the sternoclavicular, acromioclavicular and acromiohumeral joints. Thus, when the shoulder moves, a certain amount of movement occurs in all these joints and joints.
Head of humerus articulates with a small oval-shaped articular cavity of the scapula, along the edge of which a fibrocartilaginous ring is located to increase the area of contact and strengthen the joint. An articular fibrous capsule is attached to its posterior edge. Below, the joint capsule is attached to the neck of the humerus; it is relaxed (increased in volume), which causes significant mobility of the shoulder joint. The inner (synovial) membrane lines the joint and forms two bags (protrusions), through which two muscles penetrate into the joint cavity: the subscapularis and the tendon of the long head of the biceps brachii muscle.
Shoulder joint It also strengthens the so-called rotator cuff, which includes the following muscles: in front - the subscapularis, behind - the infraspinatus and teres minor, and above - the supraspinatus.
During class sports movements in the shoulder joint are performed with maximum amplitude and very high angular velocity, which predisposes the joint to injury (Sobel). In addition, frequent overhead movements with high speed and large amplitude can lead to the development of chronic injuries (Hawkins, Hobeika).
As the results show research, during sports activities the shoulder joint is not subjected to the same loads as joints lower limbs(this refers to running and jumping disciplines), however, the reaction force in the shoulder joint itself can reach 90% of body weight when abducted by 60-90° (Freedman Munroe). Combined with high angular velocities, large ranges of motion, and repeated repetition of the same movements, this results in greater stress on the shoulder joint during certain sports.

Acromiohumeral joint plays an important role in understanding the pathophysiology of some shoulder injuries. It is often called the supraspinatus "exit". The uniqueness of this joint is that it is the only place in the human body in which a muscle or tendon is located between two bones. In this case, the rotator cuff covers top part the head of the humerus, and its - the lower part of the acromion. When playing most sports, it is the supraspinatus tendon and muscle that becomes “trapped” between the acromion and the head of the humerus; in some cases, the subscapularis and infraspinatus muscles may be “trapped.”
Except rotator cuff tendons, the supraspinous “outlet” includes the subacromial bursa and borders superiorly and medially with the coracoacromial ligament. If these structures are damaged or swollen, “strangulation syndrome” may occur in this area.
At swelling or muscle hypertrophy in the supraspinatus “exit” in an athlete, subsequent repetition of movements above the head leads to increased swelling and the development of reactive inflammation. This can lead to bone impingement, and continuous repetition can cause rotator cuff tears (Hawkins, Hubeika).
U athletes Instability of the shoulder joint is also common. This is partly due to its unique anatomy, which provides an almost “global” range of motion.
Compared to hip The stability of the shoulder joint is practically zero. The femoral head is almost completely covered by the acetabulum, providing excellent architectural stability. At the same time, less than 30% of the surface of the humeral head is occupied by the glenoid fossa, which causes insignificant stability of the joint.
As a result, the probability is quite high (96-98%). More than 96% of dislocations occur in the forward direction and only 2-3% - backward. Dislocations may recur periodically and become chronic; this is likely related to activity level. The relapse rate reaches 70-90 if the first dislocation occurred before the age of 20 years inclusive. At this age, many teenagers are actively involved in sports, so athletes often experience repeated or habitual dislocation.

Also often observed subluxations and other manifestations of shoulder instability. Since with instability, as a rule, there is no “pure” dislocation and the main symptom is pain, the athlete may not be aware of joint instability.
Finally, some athletes Shoulder instability syndrome may develop in more than one direction. This is the so-called multidirectional instability.
In the absence of inherent shoulder joint stability forced to "rely" on soft fabrics(articular capsule, ligaments and muscles) to ensure its stability. As athletes perform overhead movements through a maximum range of motion, these soft tissues are subjected to overload and excessive stretching. In addition, repeated movements in one direction affect the structures located on the opposite side of the joint, which can lead to their contraction.
Similar combination of super mobile fabrics on one side of the joint and contraction on the other contributes to instability of the joint, disrupting the symmetrical location of the head of the humerus in the glenoid fossa. The muscles of the shoulder joint are also subject to significant stress. According to scientists, such eccentric overload can cause periarthrosis in the form of tendonitis with subsequent degeneration of the tendon area.
U athletes Injury to the acromioclavicular joint may also occur, which is usually acute traumatic rather than fatigue in nature (Canale et al.). An acromioclavicular joint dislocation occurs due to a direct blow to the top of the shoulder while the arm is at the side. This type of injury occurs in American football, ice hockey, rugby, and lacrosse.
Osteoarthritis of the shoulder joint It is rarely observed in athletes, and if it occurs, it exclusively affects the acromioclavicular joint. The disease is usually secondary, often occurring after a joint dislocation. Chronic degenerative changes in this joint occur among weightlifters, boxers and hockey players who have not had acute traumatic injuries.
Sports injuries to the sternoclavicular and scapulothoracic joints are very rare. However, a “contact” injury directly to the sternoclavicular joint or the lateral part of the shoulder can lead to dislocation of the joint or fracture of the articular end of the clavicle. Sports are the second most common cause of these injuries (after car accidents). Displacement of the sternoclavicular joint backward can lead to entrapment of large vessels and trachea, which can be life-threatening for the victim.





