The release of amniotic fluid (amniotic fluid) is one of the stages of normal childbirth. Rupture of the membranes of the membranes occurs during contractions when the cervix dilates. Leaking amniotic fluid before 37 weeks can cause premature birth and other serious pregnancy complications.
Possible options for water discharge
Leakage and rupture of amniotic fluid are distinguished by the time of occurrence. Normally, the amniotic sac is opened during full-term pregnancy (after 37 weeks) with partial or complete dilatation of the cervix. At this moment, the woman is in active labor. The uterus contracts regularly as the body prepares for the birth of the baby. Such an outpouring of water is called timely and does not pose a danger to the woman and the fetus.
Delayed release of amniotic fluid is said to occur if the membranes of the amniotic sac rupture during attempts in the second stage of labor. Often the baby is born in the whole amniotic sac (“in the shirt”). This phenomenon occurs with very dense membranes and is also considered normal.
Premature rupture of amniotic fluid is a condition in which the membranes rupture before labor begins. After 37 weeks, this phenomenon is not too dangerous. In this case, labor will spontaneously start within the next few hours. If necessary, the doctor can stimulate the onset of labor with medications.
A certain danger for a woman and her baby is the rupture of water for up to 37 weeks. In this case, there is a high probability of labor starting prematurely and the birth of a premature baby. Keeping a baby in a waterless space for a long time can lead to infection and the development of serious complications.
What is amniotic fluid leakage?
When the amniotic fluid is completely released, a significant rupture of the membranes occurs. In this case, it is practically impossible to maintain pregnancy until the due date. Water leakage looks a little different. In this situation, the amniotic sac does not rupture completely, but only in one small area. Amniotic fluid comes out of the fetal bladder in small portions, drop by drop. The expectant mother may not even notice the leakage of water for the time being, attributing all symptoms to increased natural discharge.
The most dangerous is the gradual leakage of water for up to 37 weeks. In this case, even a small defect in the amniotic sac can cause infection of the fetus. In some cases, intrauterine infection can lead to the death of the child. During full-term pregnancy, the risk of infection is significantly reduced.
The value of amniotic fluid
Before talking about the problem and its possible consequences, you should understand why amniotic fluid is needed.
The main functions of amniotic fluid:
- protecting the baby from infections;
- mechanical protection of the fetus and umbilical cord from any external influences;
- metabolism between mother and child;
- maintaining constant pressure of the internal environment of the uterus;
- maintaining a constant temperature;
- creating favorable conditions for the existence of the fetus.
The composition of amniotic fluid changes throughout pregnancy. During the study, you can detect various fractions of proteins, fats and carbohydrates, minerals and vitamins, oxygen and carbon dioxide. Amniotic fluid contains immunoglobulins that protect the baby from various infectious agents. And finally, particles of desquamated epithelium, vellus hair and elements of vernix lubrication freely float in the amniotic fluid.
What happens if the amniotic fluid breaks or starts leaking? The baby will lose its most important protective membrane - an intact amniotic sac with amniotic fluid inside. In such conditions, the child will not be able to exist for a long time. Further intrauterine development of the fetus will be a big question.
Reasons
Leakage of water before full-term pregnancy can be caused by the following conditions:
- isthmic-cervical insufficiency;
- genital tract infections;
- injuries during pregnancy;
- polyhydramnios;
- multiple pregnancy;
- invasive interventions during pregnancy (amniocentesis, cordocentesis, chorionic villus biopsy).
Symptoms
Recognizing the full rupture of amniotic fluid is not difficult. In the third trimester of pregnancy, the volume of amniotic fluid is 1000-1500 ml. When most of the water recedes, it is simply impossible not to notice it. In such a situation, you must immediately call an ambulance. Further tactics will depend on the duration of pregnancy and the condition of the fetus.
Leakage of amniotic fluid can go unnoticed for a long time. Externally, the water is a clear, cloudy or slightly yellowish liquid. Amniotic fluid has its own specific smell, but it can be quite difficult to recognize it. The smell is not too strong and many women simply do not notice it.
The release of amniotic fluid, even with a slight rupture of the membranes, occurs constantly. Drops of amniotic fluid remain on underwear and bedding in the form of small round spots. When changing body position and physical activity, the amount of discharge increases. If the bladder rupture increases, amniotic fluid begins to flow down the legs.
Water leakage or another problem?
Amniotic fluid leakage is often confused with symptoms of a genital tract infection or urinary incontinence. Each of these conditions has its own distinctive features.
Vaginal discharge due to infection:
- abundant, thick, viscous;
- milky, yellow, green;
- have a characteristic unpleasant odor;
- accompanied by itching, burning and discomfort in the vagina.
Two simple methods are used to diagnose the cause of vaginal discharge:
- survey smear on the flora;
- bacteriological culture.
If pathogenic bacteria are detected in the vagina or cervix, specific therapy is carried out. During pregnancy, priority is given to local antibacterial drugs in suppositories and gels. The course of therapy is 5-10 days. After treatment, vaginal discharge should decrease or disappear completely.
Discharge due to urinary incontinence:
- liquid;
- yellowish color;
- have a characteristic pungent odor;
- may be accompanied by burning and pain when urinating.
Urinary incontinence is a common problem among pregnant women. The sphincters of the bladder do not always cope with the increased load, which leads to periodic urinary incontinence. The discharge increases with coughing, sneezing, laughing, or any physical activity. The longer the pregnancy, the more noticeable the problem becomes. If you suspect urinary incontinence, you should consult a urologist.
Discharges due to water leakage:
- liquid;
- transparent, cloudy or slightly yellowish;
- have a weak specific odor;
- increase with changes in body position;
- are not accompanied by any discomfort in the vagina.
If you suspect a water leak, you should immediately consult a doctor.
Diagnostics
There are several ways to determine leakage of amniotic fluid:
Diaper test
The easiest way to recognize a dangerous pathology at home. Before testing, you must empty your bladder and shower. After a shower, you should take a horizontal position, placing a clean and dry cotton diaper under your buttocks. Water leakage is indicated by the gradual wetting of the diaper over the next two hours.
Pharmacy test
A special test pad for determining amniotic fluid can be purchased at any pharmacy. This test distinguishes amniotic fluid from normal vaginal discharge and urine. Before using the test, you must read the instructions.
The study is based on identifying certain ingredients in amniotic fluid. These substances change the pH of vaginal discharge. Normally, vaginal secretions have a pH of 3.8-4.5. The test strip begins to react when it comes into contact with a medium with a higher pH (above 5.5).
The test is for one-time use only. Before use, you must ensure the integrity of the packaging. The test strip is attached directly to the laundry and remains there for up to 12 hours. If the pad gets wet quickly, it must be removed from the underwear immediately.
The result must be assessed in a well-lit place. When amniotic fluid leaks, green or blue spots appear on the pad. Spots can be of various shapes, sizes and intensity. With normal vaginal discharge, the pad does not change color.
An important point: the appearance of blue or green spots is possible with some bacterial infections of the genital tract. If there is any change in the test strip indicator, you should consult a doctor.
Restrictions:
- It is not recommended to test less than 12 hours after sexual intercourse and the use of any vaginal suppositories;
- Do not use the pad immediately after taking a shower;
- If itching, burning or other signs of an allergic reaction occur, you should remove the pad, change your underwear and consult a doctor.
Cytological examination
Testing is carried out by a doctor. Vaginal discharge is taken for examination. The resulting material is applied to a glass slide and examined under a microscope. The detection of rejected fetal skin cells and other specific elements in the smear indicates leakage of amniotic fluid.
Arborization smear
The test is carried out in a medical facility. For research, cervical mucus is taken and applied to a glass slide. After drying, the material is examined under a microscope. When amniotic fluid leaks, a pattern resembling fern leaves is clearly visible on the glass.
Amniotest
Testing consists of identifying a special substance - placental alpha-1-microglobulin in vaginal secretions. The presence of this element clearly indicates leakage of amniotic fluid. For examination, a tampon soaked in a special indicator is inserted into the woman’s vagina. Next, the swab is lowered into a test tube with a solution. A test with an indicator is added to the same tube. When amniotic fluid leaks, a colored stripe appears on the test.
Complications
Leakage of amniotic fluid can lead to the start of labor at any stage. The shorter the gestation period, the harder it will be for a premature baby to adapt to new living conditions. It is not always possible to stop labor when the water breaks.
Rupture of the membranes of the amniotic sac and prolonged leakage of water can cause infection of the fetus. In this case, the child is born with various developmental pathologies and damage to internal organs. Sudden fetal death from infection is possible at any stage of pregnancy.
What to do?
If leakage of amniotic fluid is suspected, the expectant mother must be hospitalized in a hospital. Further tactics will depend on the duration of pregnancy, the general condition of the woman and the fetus.
After 37 weeks, when water leaks, obstetricians stimulate labor. Keeping a baby in a waterless space for a long time can lead to infection. There is no point in waiting in this case. A baby born after 37 weeks is considered full-term and can exist outside the mother's womb.
If the pregnancy is up to 37 weeks and there are no signs of fetal infection, expectant management is used. Therapy is prescribed aimed at maintaining pregnancy and reducing uterine tone. The fetal lungs are prepared for independent breathing with the help of hormonal drugs.
There is no specific treatment that can stop water leakage. To assess the baby's condition, ultrasound, Doppler and CTG are regularly performed. In case of severe fetal suffering, early delivery is performed.
The nature of vaginal discharge changes several times during pregnancy. Under the influence of hormones and other factors, they become sometimes transparent, sometimes whitish, sometimes liquid, sometimes thick, and sometimes even normally they can be beige or brown. Of course, the expectant mother has to be a little nervous until she makes sure that this is how it should be.
But it is not without reason that doctors urge you to contact them if the slightest alarming or incomprehensible signs appear. Because very often, vaginal discharge during pregnancy is evidence of pathological processes that require urgent medical intervention.
Gynecologists also consider leakage of amniotic fluid to be such conditions. If you notice that your underwear is systematically wet and damp from vaginal discharge, then you should definitely make sure that it is not leaking water.
Normally, the rupture of amniotic fluid accompanies the onset of labor. At the moment of the strongest contraction, the cervix opens and the amniotic sac bursts, after which the waters immediately recede. Sometimes this happens even before the contractions begin, and then the pregnant woman should go to the maternity hospital immediately, without waiting for the contractions to begin.
However, it often happens that water begins to leak in small portions long before the due date. First of all, this indicates that the integrity of the fetal bladder is compromised, which means that the sterility inside it is now at risk. The closer to childbirth this happens, the more favorable the medical prognosis will be.
Leakage of amniotic fluid threatens the development of intrauterine infections that can reach the baby through cracks formed in the bladder. If you do not notice or miss the leakage of water in time, then in the later stages labor may begin prematurely, and in the early stages the pregnancy may be terminated or the fetus will die in utero. In addition, the risk of poor labor detail increases in the event of labor, as well as the occurrence of infectious complications in the mother.
This is why it is very important to be able to recognize leakage as early as possible. And we must admit that this can be difficult to do...
How to detect water leakage during pregnancy
Amniotic fluid, as a rule, does not have a characteristic color or a specific smell by which it could be unmistakably recognized. It is completely transparent, although it may still have a yellowish tint, which further confuses expectant mothers (and in case of pathologies - green), and contain flakes of vernix lubrication.
The greatest difficulty is that leakage occurs in small portions, and it can be very difficult for women to distinguish: is it urinary incontinence, vaginal discharge or amniotic fluid - what does leakage look like?
There are few signs of amniotic fluid leakage. Mainly this feeling of moisture in the perineum: a woman notices that from time to time a certain amount of fluid leaks from the vagina, which is why her underwear becomes wet all the time, she has to change it often and use panty liners. Discharge during leakage occurs or intensifies when the vaginal muscles are tense: after sneezing or coughing, prolonged laughter, when a woman stands up or lifts something heavy.
But such symptoms do not always indicate that there is a guaranteed water leak. Similar signs are characteristic of urinary incontinence, which often happens in late pregnancy. It may also be normal vaginal discharge. Therefore, without additional research, it is impossible to accurately determine whether water is leaking.
Test for leakage of amniotic fluid
If there is a suspicion of leakage of amniotic fluid, then the simplest and most affordable thing a pregnant woman can do in such a situation is to buy and carry out a special leak test. It contains a pad impregnated with a reagent that only reacts to substances with a high pH level, like amniotic fluid. If the color of the pad changes while wearing it, you should immediately consult a doctor. Detailed instructions on how to conduct a leak test at home are included in each amnitest package.
Analysis for leakage of amniotic fluid
A more reliable result can be obtained by passing amniotic fluid leak test. To do this, you need to visit a gynecologist, and he will take a smear from the vagina. If the smear reveals cells contained in the amniotic fluid, the leak will be confirmed.

Will an ultrasound show leakage of amniotic fluid?
In fear of the worst outcome and possible consequences, pregnant women are ready to undergo any examination to make sure that everything is in order. In this regard, many women are interested in whether they will see leakage of amniotic fluid on an ultrasound.
The fact that the wall of the fetal bladder, through which the amniotic fluid is released, is not intact, is not visible on ultrasound. However, a specialist will certainly diagnose low water, one of the reasons for which may be prolonged leakage of water. Carrying out an ultrasound examination over time can confirm the leakage of amniotic fluid if its amount decreases.
At what age can amniotic fluid leak?
Most often, pregnant women begin to suspect leakage in the later stages, especially when there is less and less time left until the expected date of birth.
During this period, the risks of the amniotic sac losing its integrity increase, and the woman herself becomes more and more suspicious and worries about every occasion and even without. However, trouble can happen at an earlier date.
Water leakage in early pregnancy
This doesn't happen often, and it's even rarer that it can be detected. This means that not every experienced doctor is able to diagnose leakage of amniotic fluid in the early stages of pregnancy or even suspect it. After all, the amount of amniotic fluid during this period is still insignificant, and vaginal discharge is usually abundant, watery and transparent. Leaking in tiny portions, the water mixes with leucorrhoea and thus “hides”. Difficulties in diagnosis often lead to pregnancy being terminated in the early stages for this reason.
In most cases, water begins to leak in the late stages of pregnancy. This significantly increases the chances of its preservation. But you still need to understand that it is somehow impossible to stop the process. If there is little time left before the expected date of birth, and the child is ready to be born without serious consequences for his health, then doctors will most likely decide on an emergency birth: they will perform an induction or a caesarean section. Otherwise, the mother will be admitted to the hospital for safekeeping and will be prescribed therapy that will reduce the risk of intrauterine infection of the child and help her safely wait until the baby’s lungs and other vital organs mature enough to allow for early delivery.

Water leakage during pregnancy: causes
From the very beginning of its development, the future baby is reliably protected from possible negative influences of the outside world. One form of this protection is a sealed amniotic sac filled with sterile amniotic fluid. Here, in a small, cozy home for the baby, the necessary conditions for its favorable development are preserved and maintained.
As the baby grows, the amount of amniotic fluid increases, providing, among other things, the nutrition the baby needs and the environment for comfortable movement. And if the water begins to leak, then this only means one thing: the integrity of the fetal bladder is compromised, which, of course, should not be normal. But there may be several reasons leading to thinning of the bladder walls, ruptures and microcracks:
- bad habits during pregnancy;
- infectious diseases, including genitourinary infections suffered by the expectant mother, inflammatory processes in the vagina or uterus (most often leakage occurs due to colpitis, endocervicitis);
- some chronic diseases of a pregnant woman;
- isthmic-cervical insufficiency (when the cervix is not able to hold the fetus inside the uterus properly);
- carrying multiple pregnancies;
- polyhydramnios;
- trauma during pregnancy;
- neoplasms on the uterus;
- pathologies of the structure of the uterus or pelvic bones (most often a narrow pelvis during pregnancy);
- puncture of the amniotic sac prior to leakage (for example, after amniocentesis, cordocentesis or chorionic villus sampling).
For whatever reason, trouble happens, you always need to act the same way. If amniotic fluid begins to leak, then without medical supervision there is practically no chance that the pregnancy will end successfully. Be sure to tell your doctor if something confuses or worries you: competent medical support will help the baby be born without any risks.
If premature rupture of amniotic fluid occurs, you must urgently go to the hospital!
Especially for - Larisa Nezabudkina
A pathological condition caused by high rupture of the membranes or the formation of microcracks in them. It is manifested by the constant release of a small amount of watery amniotic fluid. For diagnosis, examination with mirrors, amniotests, amniocentesis with a safe dye, examination of a vaginal smear under a microscope, and transabdominal ultrasound are used. Obstetric tactics are determined by the duration of pregnancy, the condition of the mother and fetus, and the presence of complications. During expectant management, antibiotics, glucocorticoids, and tocolytics are prescribed. Active tactics include termination of pregnancy or induction of labor.

General information
Damage to the ovum with minor leakage of water is observed in almost half of the cases of premature rupture of the amnion. According to various authors, this pathological condition occurs in 2-5% of pregnancies and is the cause of almost 10% of perinatal mortality cases. Due to minimal clinical manifestations, leakage is often not detected in time, which significantly increases the risk of infectious and other complications. It is the rupture of the membranes that provokes premature birth and is the main cause of prematurity, pulmonary hypoplasia and fetal sepsis - three key factors that increase the risk of death of the newborn. The use of modern diagnostic methods and rational management of pregnant women with damaged membranes can significantly improve the prognosis for mother and child.

Causes of amniotic fluid leakage
The constant release of a small amount of amniotic fluid is observed when the integrity of the fetal membranes is damaged. In contrast to abundant premature rupture of amniotic fluid as a result of rupture of the lower pole of the ovum, leakage usually occurs with the so-called high lateral tear or the formation of microcracks. There are several groups of reasons leading to damage to the amniotic membrane:
- Infectious processes. Spontaneous rupture of fetal membranes is more often observed in pregnant women suffering from endometritis, colpitis, cervicitis, adnexitis. The strength of the amnion is significantly reduced with chorioamnionitis.
- Disorders in the uteroplacental system. The likelihood of damage to the amniotic sac increases in the presence of a bicornuate or double uterus, ICI, placental insufficiency, membrane attachment or premature placental abruption.
- Iatrogenic effects. Leakage of water can result from repeated bimanual examinations, transvaginal ultrasound, amniocentesis, chorionic villus sampling, and cervical reinforcement with ICI sutures.
- Fetal factors. The walls of the amniotic bladder experience increased pressure during multiple pregnancies, hydrocephalus of the fetus, anomalies of its position and insertion of the presenting part.
- Pathology of the membranes. Excessive distension of the amnion occurs with polyhydramnios, caused by primary and secondary hyperproduction of amniotic fluid or impaired resorption. The elasticity of the membranes also decreases with their hyaline degeneration (premature degeneration).
- Abdominal injuries. The membranes of the fetus can rupture due to a sharp blow to the abdomen or penetrating wounds to the abdominal cavity and uterus.
Treatment of amniotic fluid leakage
When detecting water leakage in a woman with a 34-36 week pregnancy, both expectant and active tactics are used. Since there is no reliable evidence that induction of labor at this stage worsens neonatal outcome, the second option is preferable. Waiting often provokes the development of chorioamnionitis and compression of the umbilical cord. The duration of observation usually does not exceed 1 day. After the onset of labor, antibiotics are prescribed for prophylactic purposes.
At 37 or more weeks of gestation, if amniotic fluid is detected in the discharge and labor is absent, induction of labor is indicated. Antibacterial therapy is used in the diagnosis of chorioamnionitis. Preventive antibiotics are recommended only in cases where the expected duration of water leakage exceeds 18 hours.
Prognosis and prevention
The prognosis for leakage of amniotic fluid depends on the duration of pregnancy. The rational use of expectant management allows the fetus to mature as much as possible and minimizes the risk of infectious complications. Stopping leakage during a 22-33 week pregnancy allows you to prolong it to full term if the condition of the woman and fetus is satisfactory and the amount of amniotic fluid remains at a normal level. If water leakage continues, there are no signs of inflammation, and the condition of the pregnant woman and fetus is satisfactory, prolongation is possible for no more than 1-3 weeks. The risk of perinatal mortality decreases significantly with preterm birth from 31-33 weeks of pregnancy, and the incidence of newborns - from 34 or more. Prevention of premature leakage of water involves limiting heavy physical activity, quitting smoking, timely registration and regular visits to an obstetrician-gynecologist, justified prescription of invasive diagnostic procedures (especially when risk factors are detected).
Amniotic fluid is not just a layer of water that protects the fetus from trauma and allows the baby to move freely. Without amniotic fluid (and even if it is present, its amount is less than normal), the child cannot fully develop. Therefore, a woman should know how to determine leakage of amniotic fluid by simple symptoms and with the help of home tests.
Amniotic fluid is formed from the moment of conception. Their number gradually increases, reaching a peak in the second trimester. By the time of birth, amniotic fluid is not formed as intensively. Water leakage during pregnancy can occur at any stage. Before 22 weeks this is a sign of an incipient miscarriage, after which it is a sign of the onset of labor.
Why does amniotic fluid leak?
The reasons for leakage of amniotic fluid at different periods are different. Depending on this, the tactics for managing a pregnant woman are built.
At the beginning of gestation
At this time, isolated leakage of amniotic fluid is rarely observed. More often, a miscarriage begins with bloody discharge and only then, as the uterus contracts and the fertilized egg is expelled, amniotic fluid is released. It mixes with blood and is difficult to isolate separately.
In the middle and end of gestation
Even the slightest leakage of amniotic fluid before 22 weeks is considered the beginning of a miscarriage. After this period and up to 37 weeks, the release of amniotic fluid is a signal of the imminent onset of premature labor. However, even at this time the prognosis in many cases is not entirely favorable. After 37 weeks, the appearance of amniotic fluid is considered normal and indicates the beginning of labor.
Leakage of amniotic fluid occurs for various reasons, which cannot always be determined even after a thorough examination. The main ones include the following:
- Infectious diseases. Sexual infections and the TORCH complex (recent rubella, cytomegalovirus, herpes) are the cause of premature leakage of amniotic fluid in the first and second trimesters in 95% of cases. When the source of inflammation is localized in the vagina and cervix, pathogens penetrate further into the cervical canal, uterine cavity, and fetal membranes. Infection of the membranes is the cause of premature rupture of amniotic fluid.
- Chronic processes. Serious chronic diseases, for example, pyelonephritis, autoimmune pathologies can also indirectly cause rupture of water.
- Rhesus conflict. When the blood groups of the fetus and mother are incompatible according to the Rh factor, Rh sensitization occurs. In such a situation, the body tries to “get rid” of an unwanted pregnancy, which causes water leakage.
- Multiple pregnancy. When carrying two or more fetuses, a woman has an increased risk of developing premature birth due to excessive stress on the body. Often multiple pregnancies are accompanied by isthmic-cervical insufficiency of the cervix (ICI, opening of the cervix prematurely). With monochorionic twins or triplets (one placenta for all), “steal syndrome” may occur. As a result, one baby develops polyhydramnios, while another develops oligohydramnios. All this is often accompanied by leakage of amniotic fluid.
- Pathology of the cervix. ICN leads to premature rupture of water. In this case, as the pregnancy period increases, the cervix cannot withstand the load and begins to open. The result is that the amniotic sac prolapses (sinks) into the cervical canal and ruptures.
- Cervical manipulation. When applying an obstetric suture for cervical incompetence, accidental puncture of the amniotic sac may occur, followed by rupture of water.
- Diagnostic procedures. Amniocentesis (puncture of the uterus through the anterior abdominal wall and collection of a small amount of amniotic fluid), cordocentesis (umbilical cord puncture for blood collection or transfusion), chorionic villus biopsy (the procedure is similar to amniocentesis, but chorionic cells are collected) due to their invasiveness are always accompanied by risks water leakage
- Uterine fibroids. In the presence of several myomatous nodes or even one large one, the extensibility of the myometrium decreases. And after 12-16 weeks, intensive growth of the uterus begins. If the nodes “interfere” with this, the pressure breaks the integrity of the membranes and water leaks.
- Anomalies of the structure of the uterus. In this case, a similar picture develops as with nodes. A uterine septum, one horn, or saddle can lead to rupture of water.
- Fetal pathology. If the baby has any developmental defects, the likelihood of water breaking before full-term pregnancy occurs is also higher.
- Injuries. Injuries in the abdominal area (blunt, sharp) can lead to compression of the amniotic sac and rupture of the membranes.
- Thrombophilia. Changes in the properties of connective tissue and blood lead to destructive transformations of the cervix and membranes, which provoke rupture of the membranes.
- Diabetes mellitus. Changes in metabolism, especially with decompensation of sugar, increases the risk of premature birth and leakage of amniotic fluid.
Premature birth sometimes occurs due to specific circumstances, for example, infection, fetal pathology. But often no obvious reasons for the early onset of labor are found.
What does it look like
Amniotic fluid leakage can look different. It all depends on the level of tear.
- Heavy and medium discharge. When the bulk of the amniotic fluid flows out, which is located in front of the presenting part of the fetus (like a “wedge”), the woman notes that it “flows down the legs”; ordinary maxi pads cannot absorb all the amniotic fluid.
- Minor discharge. When there is a high tear in the amniotic sac or when the layers of the membranes are displaced relative to each other, the defect area may overlap and the amniotic fluid stops leaking. In this case, the amount of water may be insignificant - up to 200 ml or less. In such a situation, it is sometimes difficult to diagnose and confirm whether it was amniotic fluid or not.
- Color and presence of impurities. Amniotic fluid may contain blood (in this case it is necessary to exclude placental abruption), with an admixture of meconium - green or yellow (a sign of fetal hypoxia). Normally, the color of amniotic fluid when leaking should approach transparent, with a milky tint; it may contain fetal vellus hair and particles of its epithelium - all this provides a kind of suspension.
- Smell . Amniotic fluid does not have a pungent odor, perhaps a slight sour odor. Fetid, unpleasant - a sign of infection of the membranes and, most likely, the baby.
- With or without contractions. Water can leak with or without the onset of uterine contractions and contractions.
Leakage can occur both after physical activity and during well-being, for example, during sleep or after a night's rest. When your body position changes, amniotic fluid may flow more abundantly.
So, the main symptoms of amniotic fluid leakage are as follows:
- increased amount of vaginal discharge;
- liquid discharge;
- appear periodically or leak constantly.

How to understand what kind of discharge it is
In a premature pregnancy, it is extremely important to distinguish true leakage from normal vaginal leucorrhoea. This is not always easy to do without additional examination and follow-up. It is especially difficult to make a diagnosis in the following cases.
- For urinary incontinence. Even in young women, especially after repeated births, the tone of the pelvic floor muscles can decrease, resulting in urinary incontinence - when straining, sneezing, coughing. This is especially common in the later stages, when the uterus creates additional pressure on the bladder and pelvic floor. If the pregnant woman does not notice this, it may seem like water is leaking.
- With a pessary installed. After installation of a RAP (unloading obstetric pessary) - a foreign body - the amount of vaginal discharge increases due to constant inflammation. They collect in the posterior fornix and can flow more abundantly when turning the body. Sometimes it seems like it's water.
- For inflammation in the vagina. An infectious process in the vagina is always associated with an increase in the amount of discharge. Depending on the nature of the inflammation, they may be transparent, white, yellow or green.
- When the mucus plug comes out. As the moment of birth approaches and the cervix opens, mucus comes out, which during pregnancy “like a plug” closes the cervical canal from infection. Sometimes it has a rather thin consistency and can resemble water.
The following table shows what signs can be used to differentiate water leakage from other conditions.
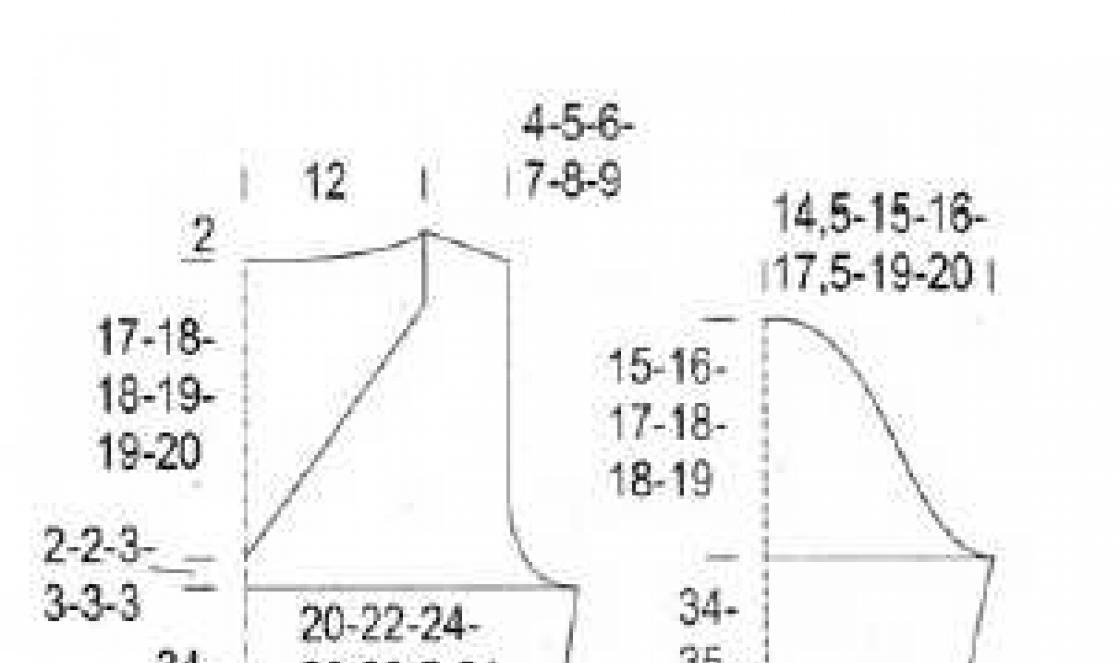
Table - How to distinguish water from other secretions
| Criterion | Water | Discharge during pessary | Discharge due to inflammation | Mucus plug |
|---|---|---|---|---|
| Quantity | Usually a lot | Enough panty liner for personal hygiene | Sparse | |
| Color | Normally transparent, but may be bloody, green or yellow | Most often white or yellowish | Depending on the cause of inflammation - from transparent (with vaginosis) to yellow, white, curdled | Transparent, but there may be streaks of blood, whiter than the vagina |
| Smell | Usually no, but with inflammation an unpleasant putrefactive | Sour, often unpleasant | “Fishy” for vaginosis and purulent, putrefactive – for other types of inflammation | Doesn't have |
| Consistency | Watery | Creamy | Thickish | Like egg white or thicker |
| Appearance time | Suddenly | 2-3 weeks after installation of the pessary | No pattern | Before childbirth, including premature |
| Do they pass | Only with high bubble tear | After removal of the pessary and sanitation | After treatment | They no longer go away before childbirth, but may decrease somewhat. |
In order to recognize leakage of amniotic fluid and distinguish it from other conditions, the following is done.
- Inspection in the mirrors. In most situations, when examining the mucous membrane of the vagina and cervix in gynecological mirrors, it is possible to understand whether it is water or just discharge.
- Smear. With a positive analysis, after staining the discharge, a “fern symptom” is detected - under magnification after drying, the picture on the slide resembles the leaves of this plant.
- Amniotest. There are special test strips to determine the presence of amniotic fluid. They are based on changes in the pH of vaginal discharge when mixed with amniotic fluid. It is freely sold in pharmacies, and a woman can perform it herself at home.
- Ultrasound of the fetus. If oligohydramnios is detected by fetal ultrasound, if rupture of amniotic fluid is suspected, this is another “for” symptom. However, a normal amniotic fluid index does not exclude leakage, especially a high tear.
- Laboratory methods. Some clinics have methods for identifying certain substances in vaginal secretions, which appear only after amniotic fluid enters them. However, the method is expensive and not always informative, so it is rarely used.
In doubtful cases, wait-and-see tactics are used. The woman is being monitored in a hospital setting. Careful monitoring of discharge is carried out, ultrasound is performed in dynamics, tests and laboratory studies are performed.
Management tactics for pregnant women with leakage
If signs of amniotic fluid leakage are obvious or there is reliable confirmation of this process, the pregnant woman undergoes a series of examinations, after which further management tactics are established. It largely depends on the period in which the waters began to flow.
- 1st trimester. Bloody discharge and water in this period begin together when the integrity of the amniotic sac is disrupted and the miscarriage progresses. Medical or surgical termination of pregnancy is indicated.
- 2nd trimester. Before 22 weeks, any leakage of amniotic fluid is considered the onset of a miscarriage. Further stimulation is carried out and subsequent curettage of the uterine cavity.
- 3rd trimester. Tactics are determined based on the period, condition of the mother and fetus. When the waters rupture before 37 weeks, it is possible to prolong pregnancy from several days to a month or even more with simultaneous antibiotic therapy and the administration of drugs for the maturation of the fetal lungs. There are techniques to prevent further leakage of amniotic fluid, which helps to grow the baby in utero for some more time. Since water is produced anew every four to eight hours, its volume soon increases to normal levels. If there are signs of detachment, inflammation, or according to the woman’s indications, delivery can be immediate. The rupture of water after 37 weeks is equivalent to the onset of labor.

Is it dangerous for the fetus?
The rupture of water during full-term pregnancy is most often accompanied by the onset of active contractions in the next day. Therefore, at this time it is the least dangerous. When amniotic fluid leaks from 22 to 37 weeks, the severity of the baby’s condition is determined by the cause that led to this, as well as the degree of leakage of water. The most favorable prognosis is with a high tear of the bladder without concomitant inflammation. In all other cases, the rupture of water ends in premature birth.
The consequences of water leakage for a child ahead of schedule are as follows:
- the risk of infectious complications increases– chorioamnionitis, congenital pneumonia;
- hypoxia occurs– rupture of water affects the uteroplacental blood flow, especially if it occurs against the background of any diseases of the woman;
- there is a possibility of being born prematurely– if water breaks in the early stages, it is difficult (up to 30-32 weeks) to keep a pregnant woman for more than a month;
- Parts of the fetal body may fall out - with a non-cephalic presentation, along with the water, loops of the umbilical cord or parts of the fetus (usually arms, legs) may fall out through the opened cervix, which can threaten its life.
If a woman is able to suspect or even accurately determine leakage of amniotic fluid at home, then the sooner she seeks medical help, the better, since a condition without amniotic fluid is dangerous for the fetus. It doesn’t matter what the gestational age is when water breaks, only a specialist can determine the most appropriate tactics in each specific case.
Another serious problem that can happen during pregnancy is leakage of amniotic fluid. This can lead to major complications both during pregnancy and during the birth itself.
Amniotic fluid, or more precisely amniotic fluid, plays a significant role in the development of the fetus. Any change in its composition and quantity has great consequences, because amniotic fluid is not only the habitat of the unborn baby, but also protection from various infections and external influences, its nutrition and a means of facilitating the pregnancy process for the woman herself.
The volume of amniotic fluid increases in direct proportion to the development and growth of the baby. Thus, if in the first trimester there is about 6-11 ml of amniotic fluid, then already in the second trimester it is 260-290 ml. In the last trimester, amniotic fluid should normally be 1.2-1.5 liters. But before the birth itself, their volume decreases by 2 times. In this regard, two problems may arise: oligohydramnios and polyhydramnios.
In addition, amniotic fluid performs the following functions, the incorrect implementation of which can lead to serious problems:
- saturation of the fetus with special nutrients that are contained only in the amniotic fluid;
- maintaining constant pressure;
- maintaining a normal temperature no higher than 37 degrees (if the future parent is not sick);
- protection of the fetus and child's place from shocks and compression from the outside;
- protection against infections due to the presence of immunoglobulins in the amniotic fluid;
- ensuring freedom of movement of the fetus;
- protection from strong noise produced outside.
Normally, such useful amniotic fluid should flow out only during labor, both naturally and during labor stimulation with puncture of the amniotic sac.
If amniotic fluid leaks before labor occurs, then the body signals to us that the pregnancy is proceeding with abnormalities that must be carefully examined and monitored.
Signs of amniotic fluid leakage
As simple as it may sound, leakage of amniotic fluid is often difficult to notice and identify immediately. Quite often it is confused with simple urinary incontinence or various secretions, the volume of which increases with the duration of pregnancy. That is why you need to tell your doctor about everything in order to prevent leakage of water and to be safe from various complications during pregnancy. But you should also pay close attention to this type of discharge and study it carefully, because amniotic fluid does not have the color and characteristic odor that is present in urine, and also does not have a mucous base, like vaginal discharge.
If you suspect leakage of amniotic fluid, you can do a rapid test at home. To begin with, you will have to empty your bladder as much as possible, wash yourself thoroughly and wipe yourself dry. Next, you will need to lie down on a completely clean and dry sheet for about 15 minutes. If the sheet becomes even a little wet, you should immediately call an ambulance.
If water leakage is missed during the first trimester, then in 90% of such cases abortions are subsequently necessary.
If at the very beginning of pregnancy it is difficult to notice water leakage, then at a later stage, about 2 weeks before birth, it is impossible not to recognize it, because up to 500 ml of amniotic fluid flows out immediately. Usually after this, contractions begin immediately.
In order not to miss the leakage of amniotic fluid and to recognize it in time, during pregnancy you should give preference to light-colored cotton underwear and regularly use panty liners, which will allow you to track the frequency of discharge.
Remember that if, with urinary incontinence, it is released when laughing, coughing, sneezing, then amniotic fluid does not depend on this, and if it leaks, then just like that, without external factors, which is what the home rapid test is based on. 
How to detect leakage of amniotic fluid
Leakage of amniotic fluid occurs due to damage to the lining of the uterine walls. The stronger the cracks and breaks, the more fluid leaks out. Also, the volume of amniotic fluid leaked is affected by the height of the uterine fundus.
Thus, if the cracks are very small, then very little amniotic fluid is lost, and this loss is quite difficult to notice. And to notice such water leakage, 4 methods were created:
- Smear microscopy. Dried amniotic fluid crystallizes and forms a pattern similar to fern leaves. If, during analysis, such a pattern is obtained on the glass, then water is leaking.
- Nitrazine test. This test determines the pH of the vagina. If, according to analysis, the vaginal environment is neutral or slightly alkaline, then water leakage occurs; normally, the environment should be acidic. This analysis can be performed at home, and the test itself is easily sold in pharmacies.
- Protein-1 test. This analysis looks for a specific type of protein that is found only in amniotic fluid.
- α-microglobulin-1 test. This element is also found only in amniotic fluid. It is quite easy to detect when water leaks due to its significant content in them.
The first 2 analyzes do not always give the correct result, because... The reaction can be affected by various components of urine, vaginal discharge, and sperm residues. In addition, the more time has passed since the uterine membranes ruptured, the less informative these tests will be.
The clearest and most accurate results will be given by tests for protein-1 and a-microglobulin-1. In such tests, various secretions are easily distinguished from amniotic fluid. In addition, for these studies, special monoclonal antibodies were invented that do not react to any other types of discharge except amniotic fluid.

Cause of water leakage
As noted above, leakage of amniotic fluid occurs due to cracks and tears in the lining of the uterine walls. Why are they formed?
- Infections that affect the amniotic fluid, as well as inflammation of the genital organs of a pregnant woman. This reason most often occurs during premature pregnancy. The cervix ripens ahead of time, as a result of which certain substances are released that help soften the membrane of the fertilized egg and placental abruption. This is very dangerous for the expectant mother and her child, not only for their health, but also for their life in general, because can lead to fetal hypoxia and uterine bleeding.
- Incorrect position of the fetus and the narrow pelvis of the woman in labor. Here, water leakage is not so dangerous, because... occurs already during the birth itself, but it complicates and slows it down, the uterus opens very slowly. And due to the fact that most of the water ends up in the lower part of the bubble, the shells are severely torn.
- Cervical insufficiency, otherwise known as isthmic-cervical insufficiency. The amniotic sac protrudes, making the lower part easily susceptible to various infections, and any even minor physical activity can lead to its rupture. This deficiency affects 25% of pregnant women in the last trimester.
- Bad habits: alcoholism, smoking, drug addiction.
- Various diseases of women, such as anemia, connective tissue diseases, weight loss.
- Multiple pregnancy.
- Abnormal development of the uterus (short cervix, presence of a uterine septum) and fetus.
- Such serious diseases as colpitis, tumors on the body of the uterus (malignant and benign), endocervicitis.
- The pregnant woman underwent additional tests, such as amniotic fluid collection or chorionic villus sampling.

What is the effect of leakage of amniotic fluid?
The type and degree of complication is influenced by the time at which the leak was discovered, as well as how soon it was identified and taken under the control of the attending physician. Leakage of amniotic fluid can lead to the following:
- Abnormal labor: extreme weakness during labor, prolonged labor, or, conversely, too rapid labor. Both have a negative impact on both mother and child.
- Premature placental abruption and severe bleeding, which can lead to pituitary ischemia or uterine amputation.
- Complications of infectious and inflammatory processes in the unborn baby and his mother, which occur in a quarter of women giving birth due to intra-amniotic infection. Also, in 12%, complications continue after childbirth, resulting in postpartum endometritis.
- Serious complications for the fetus: hypoxia and asphyxia. Subsequently, ischemic encephalitis or pancreatitis may develop, the treatment of which is quite complex and lengthy, if it is possible at all.
- Respiratory distress syndrome. It occurs most often during premature birth, when the baby’s lungs are not yet fully formed and cannot collapse due to a lack of surfactant.
All consequences of leakage of amniotic fluid are very serious and dangerous, which requires immediate contact with your doctor and the appointment of high-quality treatment. First of all, such problems require antibacterial therapy in the early stages so that infections do not have time to reach the uterine cavity and fetus. If the timing is later, and the baby is almost formed, then if there is leakage of amniotic fluid, there is only one purpose: artificially inducing labor.
It is very important to see a doctor in time and start treatment, in which case the pregnancy can still be saved. If you are not attentive to the problem that has arisen, then the pregnancy will have to be terminated due to too great a threat to the life of not only the unborn baby, but also the mother.

How to deal with water leakage
Like the consequences of leakage of amniotic fluid, the choice of treatment for this dangerous disease depends on the degree of damage to the walls of the uterus and the volume of amniotic fluid leaking.
- In the first trimester, if they do not have time to notice the leakage of amniotic fluid, then in 90% of cases the matter is resolved by abortion.
- In the second and third trimesters, the attending physician prescribes hospital treatment for the pregnant woman. The hospital is constantly monitoring the health of the expectant mother and her baby, and the development of the situation. At this stage, every day the baby lives in the womb without incident is very valuable and has a great influence on the full development of the fetus. The closer the natural and full-term birth is, the healthier and stronger the baby will be born. If a large amount of amniotic fluid has leaked, but another 6 hours have not passed after this, then the attending physician prescribes antibiotics to the pregnant woman, which prevent infection of the fetus in the absence of amniotic fluid protection.
- If leakage of amniotic fluid develops (volume and frequency increases) and will soon lead to rupture of the bladder, then the doctor will urgently prescribe an artificial resolution of labor. If, after a special puncture and leakage of amniotic fluid, contractions have not begun within three hours, then special drugs are administered intravenously to stimulate labor, as well as accelerate the ripening of the cervix. But, most often, if labor does not begin, then an unplanned caesarean section is performed.
Remember that if amniotic fluid leaks, a pregnant woman will not be able to do anything on her own, so do not try to solve the problem yourself without doctors. When amniotic fluid leaks, you must strictly follow all the instructions of the attending physician and follow all the recommendations given by him.

Prevention to help protect against leakage of amniotic fluid
If, when water leaks, you cannot help yourself on your own, then you can protect yourself from this disease even before it appears by following the following recommendations:
- correct and timely preparation for pregnancy: regular visits to the gynecologist and carrying out the necessary examinations six months before planning a pregnancy, timely detection and treatment of various infections;
- proper daily routine and proper nutrition and diet;
- regular antiseptic treatment of the genital tract and other mucous membranes, basic hygiene both before and during pregnancy.
Remember, during pregnancy you need to carefully monitor your health and the slightest suspicion of discomfort should be reported to your doctor. If you have any doubts about your health, do not hesitate to ask your doctor to order additional tests if there are special indications for them. After all, even a minor illness can become a serious obstacle to the full pregnancy and birth of a healthy child.