According to research by American experts, suffer from urinary incontinence more than 12 million men. At the same time, the severity incontinence (urinary incontinence) all vary from partial to complete loss of bladder function.
And if someone loses a drop of urine while playing sports or laughing, then other men can produce large amounts and experience constant leakage, which creates serious problems.
The causes of this disease can be different. As a rule, urinary incontinence is a symptom of any pathology of the genitourinary system. It often occurs as a result of operations on the prostate gland, including radical prostatectomy. More than 10% of patients undergoing surgery for prostate cancer suffer from incontinence.
If earlier it was quite difficult to deal with this disease, now, thanks to modern treatment methods, incontinence is not a serious problem and can be gotten rid of in the shortest possible time.
So, what are the most common causes of urinary incontinence in men?
These include the consequences of operations on the prostate gland, various injuries to the brain or spinal cord, neurological diseases (multiple sclerosis or Parkinson's disease), infections of the bladder and lower urinary tract, intoxication, taking high doses of sedatives, stress or mental illness.
Types of male urinary incontinence
The most common type of incontinence is stress urinary incontinence. The cause is increased pressure in the bladder. And involuntary release of urine occurs during physical activity, laughing, coughing, or lifting weights.
Another type of incontinence is urgent (imperative, emergency) urinary incontinence. The urge to urinate is so strong that a man often cannot control it and reach the toilet. TO Urgent urinary incontinence Parkinson's disease and diabetes mellitus are often cited. Often urgent urinary incontinence is a consequence of a stroke.
Types of treatment for urinary incontinence in men
Before prescribing treatment, the doctor must find out the reasons that led to the onset of the disease. And the next step after the examination will be the selection of an appropriate treatment regimen.
Used for urinary incontinence various drug treatments, physiotherapy, and surgery.
Today, as before, physical exercises are prescribed during treatment to strengthen the pelvic floor muscles. However, this type of therapy is effective only in patients at an early stage of the disease. As, indeed, is the method of transurethral administration of the gel. It helped only 5-15% of lung patients forms of urinary incontinence .
The most effective method of treating this pathology in later stages of the disease is the installation of an artificial bladder sphincter, which allows one to defeat the disease in the vast majority of cases.
Artificial bladder sphincter AMS-800
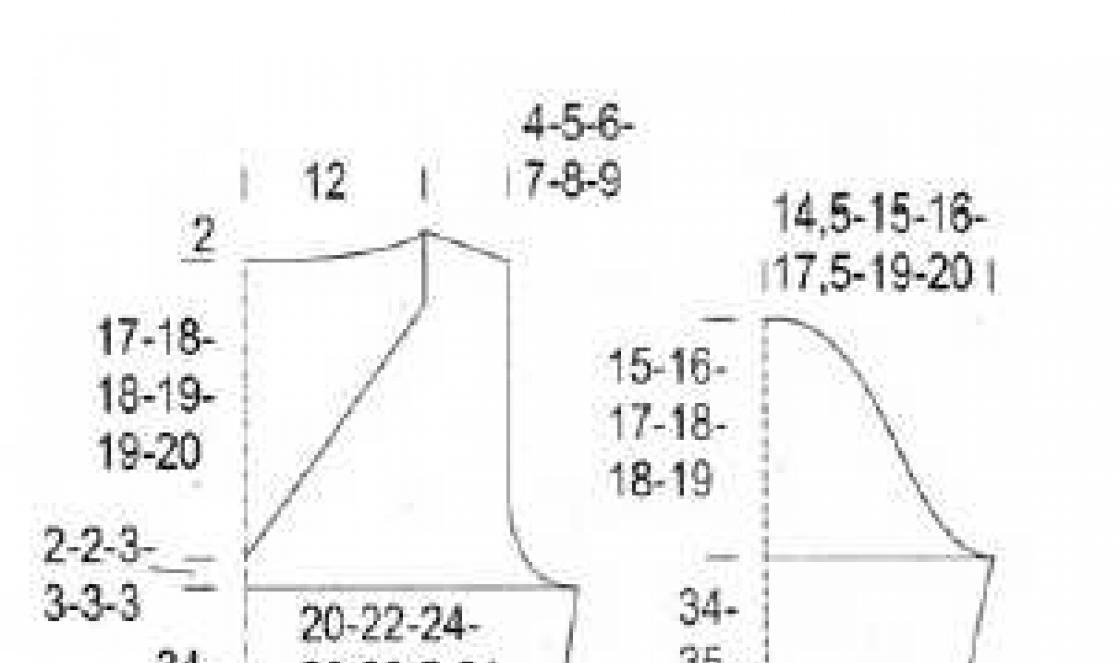
It is a silicone prosthesis consisting of an inflatable cuff (the sphincter itself), a reservoir that regulates the pressure in the sphincter and a control pump - a pump.
Artificial bladder sphincter
If the normal natural sphincter of the bladder opens during urination, but the rest of the time urine is retained and the sphincter is closed, then when the function is impaired, involuntary release of urine occurs. And the problem of bladder incompetence after illness, pelvic trauma or radiation therapy is intended to be solved by an artificial sphincter. It is installed exactly in the place where the urethra passes into the bladder.
It is the artificial sphincter that allows you to completely eliminate symptoms of urinary incontinence in most patients. The effectiveness of the method reaches 90%.

1 — sphincter cuff, 2 — reservoir, 3 — control pump, 4 — bladder,
5 - prostate gland, 6 - natural sphincter, 7 - urethra
The reservoir is placed behind the rectus abdominis muscle, and the pump itself is located in the scrotum. The sphincter wraps around the urethra. And the sphincter cuff, filled with water, compresses the urethra until the patient wants to go to the toilet. Once this happens, he presses the pump and the fluid from the sphincter flows into the reservoir. Some time after the bladder is emptied, the sphincter fills with water again and again compresses the urethra. This way urine does not leak out.
This surgery is an effective treatment for patients with partial or complete urinary incontinence. with neurological diseases, as well as after injury to the spinal cord or pelvic bones
How is the operation performed?
The sphincter is implanted through a small incision in the perineum. And the reservoir is installed from an additional incision in the groin area. The duration of the operation is about 2 hours.
And the rehabilitation period includes mandatory antibacterial therapy to exclude infection.
After the operation, the patient remains in the clinic for about a week, and a catheter is installed in the bladder for several days to remove urine.
In the future, physical activity should be limited for at least 1.5 months, depending on the patient’s condition. Until the sphincter is activated, it is also better to abstain from sex.
Your attending physician, 1-2 months after surgery, will be able to activate the sphincter and explain how to use it.
Potential risks and possible complications
In the rarest cases, infection may develop, as well as bedsores of the skin over the sphincter. In this case, the implant will have to be removed.
How it works:

Urinary incontinence: folk remedies, treatment of incontinence
Folk remedies: treatment of urinary incontinence with herbs. How to treat urinary incontinence with folk remedies. Treatment of kidney diseases with folk remedies: medicinal herbs for urinary incontinence.
BLADDER DISEASES
Causes and treatment of urinary incontinence with folk remedies. Folk remedies: what herbs to use for urinary incontinence and methods for preparing herbal medicines.
URINARY INCONTINENCE
Folk remedies

Urinary incontinence is the involuntary loss of urine in the absence of the urge to urinate.
Newborns do not know how to hold urine; this problem often arises again in old age. In women, the muscles of the uterus and pelvic floor weaken with age. This changes the angle at which the urethra (the tube leading from the bladder) passes, which contributes to urinary incontinence.
Finally, the bladder, due to frequent overflow, gradually loses tone, losing sensitivity to overflow, and loses the ability to contract and expel urine as it fills, as happens in healthy people. Urine begins to be released involuntarily, not obeying the patient’s wishes, and then it becomes difficult for him to get to the toilet on time.
Stones in the bladder can also lead to the urge to urinate very frequently and uncontrollably.
Treatment of urinary incontinence with carrot juice, a folk remedy ∗∗∗
In the morning on an empty stomach, drink 1 glass of fresh carrot juice. Take psyllium seed powder on the tip of a knife 3-4 times a day.
Undesirable products for urinary incontinence, folk remedies, treatment
Watermelons, celery, grapes, cucumbers and other foods that have a diuretic effect should be excluded from the diet.
Folk remedy: plantain infusion for urinary incontinence, treatment
Pour 1 tablespoon of large plantain leaf with 1 cup of boiling water. Infuse, wrapped, for 1 hour, strain. Take 1 tablespoon 3-4 times a day 20 minutes before meals.
Urinary incontinence: treatment with yarrow, folk remedy
Pour 1 teaspoon of finely chopped yarrow herb into 1 glass of boiling water, steam for 1 hour. Drink 0.5 cups daily 2-3 times a day before meals.
Sage in the treatment of urinary incontinence with folk remedies
Pour 40 g of dry sage herb into 1 liter of boiling water, leave, covered, for 1-2 hours. Take 0.5-1 glass 3 times a day.
Folk remedy for urinary incontinence, treatment
Pour 3 tablespoons of shepherd's purse herb with 2 cups of boiling water, leave in a thermos for 3-4 hours. Drink 0.5 cups in 4 doses before meals.
Treatment of urinary incontinence with St. John's wort and centaury, a folk remedy
Mix equal parts of St. John's wort and centaury herb. Pour 1 teaspoon of the mixture into 1 glass of boiling water and leave. Drink 2 cups a day. The course of treatment is 2-3 weeks.
Folk remedy: St. John's wort and lingonberry for urinary incontinence, treatment
Mix 2 tablespoons of St. John's wort herb and 2 tablespoons of lingonberry leaves and berries. Pour the mixture with 3 cups of boiling water, boil for 10 minutes over low heat, cool, strain. Drink in small sips from 4 pm until bedtime.
Urinary incontinence: treatment with blackberries and blueberries, a folk remedy
Mix 1 tablespoon of blackberries and 1 tablespoon of blueberries, boil in 0.5 liters of water over low heat for 20 minutes. Leave, wrapped, for 30 minutes. Drink 1 glass 4 times a day.
 Pine cone jam is a cure for all diseases.
Pine cone jam is a cure for all diseases.
Urinary incontinence

Impaired urinary continence is a common, complex problem that significantly affects the quality of life of people experiencing it. Fortunately, the current availability of high-tech surgical treatments and effective medications at the disposal of specialist doctors means that treating urinary incontinence is challenging, but not impossible. The information that will be presented below will help you navigate the problem of urinary incontinence even before visiting a urologist.
What is urinary incontinence?
Urinary incontinence refers to any involuntary loss of urine. This is not a disease, but a symptom that can be caused by a wide variety of pathologies. Urinary incontinence can occur with diabetes, multiple sclerosis, after a stroke, injuries and operations on the spine, in women with prolapse and without vaginal walls, after childbirth and operations on the uterus, in men with an enlarged prostate gland and after operations on it for benign and malignant tumors. It is generally believed that urinary incontinence is a problem for older people. Indeed, in the general population over 65 years of age, urinary incontinence occurs in 25% of women and 15% of men. However, urinary incontinence is quite common among young, socially active women.
What are the main types of urinary incontinence?
Stress urinary incontinence - is the most common type of urinary incontinence. Uncontrolled loss of urine occurs when intra-abdominal pressure increases, which can be caused by completely ordinary events (walking, laughing, coughing, sneezing, etc.). The essence of the problem is the loss of support for the urethral sphincter, even with a slight prolapse of the vaginal walls - in young women. a decrease in sphincter tone and internal urethral resistance due to a decrease in estrogen levels - in menopausal women.
In men, the most common cause is previous prostate surgery, usually radical prostatectomy for cancer, rarely transurethral resection or adenomectomy for benign hyperplasia.
Urgent urinary incontinence - the second most common type of urinary incontinence. It is observed in patients with an overactive bladder. Urinary incontinence occurs immediately following an uncontrollable urge to urinate, while the patient is unable to suppress this urge in time to reach the toilet. Quite typical provoking factors are the sound of dripping water, waking up at night and changing body position, opening the doors of your own apartment with a key. Urinary incontinence most often occurs with neurogenic bladder overactivity (stroke, multiple sclerosis, spinal injury).
Diagnostics.
As with any diagnosis of urinary incontinence, a thorough medical history and a thorough physical examination are critical. Very important aspects in the patient survey are fluid intake and toilet habits, bowel function (constipation). When collecting anamnesis, attention is paid to heredity and previous surgical interventions on the pelvic organs. The initial assessment includes a urine test, a voiding diary, and a chairside examination to detect urine loss from coughing or straining (stress test). In cases of planned surgical intervention or an unclear clinical picture, a urodynamic study is mandatory. Complex urodynamic study (CUDI) - to date, the only method that allows you to reliably assess the functional state of the lower urinary tract. This test is performed on an outpatient basis, takes about 20-30 minutes and does not cause pain.
Treatment methods for urinary incontinence.
The choice of treatment method is based on an accurate diagnosis and depends on the type of urinary incontinence.
Stress urinary incontinence Non-invasive treatments for this type of urinary incontinence include exercises to train the muscles of the perineum (known as Kegel exercises). However, we must remember that the effectiveness of this method (improvement) is no more than 70%, given that the exercises must be performed continuously for at least 6 months. For quite a long time it was believed that in all cases of stress urinary incontinence it was necessary to start with exercises and only then consider the possibility of surgical treatment. In the last decade, attitudes to this issue have been revised, and surgery is now the first line of treatment in most cases. Anterior colporrhaphy (plasty of the anterior vaginal wall) 10-15 years ago was considered by gynecologists as the main operation for the treatment of women with stress urinary incontinence. However, an assessment of the long-term results of this operation showed that its effectiveness does not exceed 50%. Currently, most gynecologists do not consider it possible to offer this method of treating urinary incontinence. For a long time, the Burch operation (pulling the vaginal wall to the pubic bones using non-absorbable sutures) was considered the “gold standard” in the treatment of women with stress urinary incontinence. Compared to modern methods of surgical correction of urinary incontinence, this method is traumatic and requires more time for recovery. However, if laparoscopic surgery is performed for diseases of the internal genitalia (for example, uterine fibroids), it is advisable to perform a laparoscopic version of the Burch operation in a patient with concomitant urinary incontinence. Currently, there is no doubt that the main operation for the treatment of stress urinary incontinence in women is the implantation of a synthetic tape in the area of the middle part of the urethra (suburethral sling), installed from the retropubic or transobturator (through the obturator foramen) position.
In men with urinary incontinence after prostate surgery, an attractive method is the injection of so-called volume-forming drugs (gels) into the sphincter area. The injections are performed under local anesthesia and can be done multiple times. Unfortunately, the effectiveness of this treatment method ranges from 10% to 30%. In recent years, specialists have shown interest in male slings. It should be noted that the different pathophysiology of urinary incontinence and the anatomical features of the male urethra and pelvis do not allow obtaining decent results. The most effective method of surgical treatment of urinary incontinence in men remains implantation of an artificial sphincter. The device consists of a cuff that is placed around the urethra, a balloon and a pump (pump) that is placed under the skin of the scrotum for patient-controlled urination.
Urgent urinary incontinence - Treatment of this type of urinary incontinence consists of conservative measures and drug therapy. First of all, you need to try to change your usual life patterns (avoid eating spices, alcohol and coffee). In general, there are no restrictions on fluid intake, but it is not recommended to drink fluid in the evening and at night. As mentioned in the section on treating stress urinary incontinence, Kegel exercises are helpful, but the patient must be committed to this type of treatment. Based on the data from the urination diary, the patient should try to restore voluntary control over urination by gradually increasing the intervals between voiding. The main treatment for overactive bladder, accompanied by urge incontinence, is to take medications that relax the bladder (anticholinergics). Vesicare, driptan, detrusitol, and spasmex are registered and approved for use in our country. Recently, generics (drugs that contain the original drug molecule, but are produced by another pharmaceutical company) have begun to appear in pharmacies. The disadvantages of anticholinergic drugs include not so rare side effects, such as dry mouth, constipation, and blurred vision. Sometimes, even with good effectiveness, some patients refuse to continue treatment due to side effects. An achievement in recent years in the treatment of urge incontinence has been the use of intravesical injections of botulinum toxin. This is especially true in patients with drug-resistant and neurogenic bladder overactivity with urinary incontinence. Finally, there is a method of implanting special devices that allow you to modulate (change) the function of the bladder. Unfortunately, due to the high cost of equipment, this method has not yet received sufficient distribution in our country.
Overflow incontinence - in these cases, the fundamental question is to determine the cause of this type of urinary incontinence. If there is an obstruction to the outflow of urine (hyperplasia, stricture disease of the urethra, etc.), the task is to eliminate bladder outlet obstruction or urine diversion. If bladder contractility is impaired, the patient requires periodic catheterization (emptying the bladder) to minimize urine loss and preserve kidney function.
What can you expect from treatment?
The ultimate goal of any treatment is to improve the quality of life of patients. And believe me, in most cases this is possible. But the result largely depends on the patient himself. Drug therapy for overactive bladder will be effective if the patient does not drink 4-5 liters of fluid per day. The positive result of surgery for stress urinary incontinence will be long-term if the patient does not gain 30 kilograms in weight. That is, long-term positive treatment results directly depend on the common sense with which the patient approaches his health.
In general, the cure rate for women with stress urinary incontinence operated on using modern techniques is close to 92%. A stable bladder condition can be achieved in 75-80% of patients with urge urinary incontinence. The effectiveness of artificial sphincter implantation operations is 70-80%.
According to research by American experts, suffer from urinary incontinence more than 12 million men. At the same time, the severity incontinence (urinary incontinence) all vary from partial to complete loss of bladder function.
And if someone loses a drop of urine while playing sports or laughing, then other men can produce large amounts and experience constant leakage, which creates serious problems.
The causes of this disease can be different. As a rule, urinary incontinence is a symptom of any pathology of the genitourinary system. It often occurs as a result of operations on the prostate gland, including radical prostatectomy. More than 10% of patients undergoing surgery for prostate cancer suffer from incontinence.
If earlier it was quite difficult to deal with this disease, now, thanks to modern treatment methods, incontinence is not a serious problem and can be gotten rid of in the shortest possible time.
So, what are the most common causes of urinary incontinence in men?
These include the consequences of operations on the prostate gland, various injuries to the brain or spinal cord, neurological diseases (multiple sclerosis or Parkinson's disease), infections of the bladder and lower urinary tract, intoxication, taking high doses of sedatives, stress or mental illness.
Types of male urinary incontinence
The most common type of incontinence is stress urinary incontinence. The cause is increased pressure in the bladder. And involuntary release of urine occurs during physical activity, laughing, coughing, or lifting weights.
Another type of incontinence is urgent (imperative, emergency) urinary incontinence. The urge to urinate is so strong that a man often cannot control it and reach the toilet. TO Urgent urinary incontinence Parkinson's disease and diabetes mellitus are often cited. Often urgent urinary incontinence is a consequence of a stroke.
Types of treatment for urinary incontinence in men
Before prescribing treatment, the doctor must find out the reasons that led to the onset of the disease. And the next step after the examination will be the selection of an appropriate treatment regimen.
Used for urinary incontinence various drug treatments, physiotherapy, and surgery.
Today, as before, physical exercises are prescribed during treatment to strengthen the pelvic floor muscles. However, this type of therapy is effective only in patients at an early stage of the disease. As, indeed, is the method of transurethral administration of the gel. It helped only 5-15% of lung patients forms of urinary incontinence .
The most effective method of treating this pathology in later stages of the disease is the installation of an artificial bladder sphincter, which allows one to defeat the disease in the vast majority of cases.
Artificial bladder sphincter AMS-800
It is a silicone prosthesis consisting of an inflatable cuff (the sphincter itself), a reservoir that regulates the pressure in the sphincter and a control pump - a pump.
Artificial bladder sphincter
If the normal natural sphincter of the bladder opens during urination, but the rest of the time urine is retained and the sphincter is closed, then when the function is impaired, involuntary release of urine occurs. And the problem of bladder incompetence after illness, pelvic trauma or radiation therapy is intended to be solved by an artificial sphincter. It is installed exactly in the place where the urethra passes into the bladder.
It is the artificial sphincter that allows you to completely eliminate symptoms of urinary incontinence in most patients. The effectiveness of the method reaches 90%.

1 — sphincter cuff, 2 — reservoir, 3 — control pump, 4 — bladder,
5 - prostate gland, 6 - natural sphincter, 7 - urethra
The reservoir is placed behind the rectus abdominis muscle, and the pump itself is located in the scrotum. The sphincter wraps around the urethra. And the sphincter cuff, filled with water, compresses the urethra until the patient wants to go to the toilet. Once this happens, he presses the pump and the fluid from the sphincter flows into the reservoir. Some time after the bladder is emptied, the sphincter fills with water again and again compresses the urethra. This way urine does not leak out.
This surgery is an effective treatment for patients with partial or complete urinary incontinence. with neurological diseases, as well as after injury to the spinal cord or pelvic bones
How is the operation performed?
The sphincter is implanted through a small incision in the perineum. And the reservoir is installed from an additional incision in the groin area. The duration of the operation is about 2 hours.
And the rehabilitation period includes mandatory antibacterial therapy to exclude infection.
After the operation, the patient remains in the clinic for about a week, and a catheter is installed in the bladder for several days to remove urine.
In the future, physical activity should be limited for at least 1.5 months, depending on the patient’s condition. Until the sphincter is activated, it is also better to abstain from sex.
Your attending physician, 1-2 months after surgery, will be able to activate the sphincter and explain how to use it.
Potential risks and possible complications
In the rarest cases, infection may develop, as well as bedsores of the skin over the sphincter. In this case, the implant will have to be removed.
How it works:

Urinary incontinence: folk remedies, treatment of incontinence
Folk remedies: treatment of urinary incontinence with herbs. How to treat urinary incontinence with folk remedies. Treatment of kidney diseases with folk remedies: medicinal herbs for urinary incontinence.
BLADDER DISEASES
Causes and treatment of urinary incontinence with folk remedies. Folk remedies: what herbs to use for urinary incontinence and methods for preparing herbal medicines.
URINARY INCONTINENCE
Folk remedies

Urinary incontinence is the involuntary loss of urine in the absence of the urge to urinate.
Newborns do not know how to hold urine; this problem often arises again in old age. In women, the muscles of the uterus and pelvic floor weaken with age. This changes the angle at which the urethra (the tube leading from the bladder) passes, which contributes to urinary incontinence.
Finally, the bladder, due to frequent overflow, gradually loses tone, losing sensitivity to overflow, and loses the ability to contract and expel urine as it fills, as happens in healthy people. Urine begins to be released involuntarily, not obeying the patient’s wishes, and then it becomes difficult for him to get to the toilet on time.
Stones in the bladder can also lead to the urge to urinate very frequently and uncontrollably.
Treatment of urinary incontinence with carrot juice, a folk remedy ∗∗∗
In the morning on an empty stomach, drink 1 glass of fresh carrot juice. Take psyllium seed powder on the tip of a knife 3-4 times a day.
Undesirable products for urinary incontinence, folk remedies, treatment
Watermelons, celery, grapes, cucumbers and other foods that have a diuretic effect should be excluded from the diet.
Folk remedy: plantain infusion for urinary incontinence, treatment
Pour 1 tablespoon of large plantain leaf with 1 cup of boiling water. Infuse, wrapped, for 1 hour, strain. Take 1 tablespoon 3-4 times a day 20 minutes before meals.
Urinary incontinence: treatment with yarrow, folk remedy
Pour 1 teaspoon of finely chopped yarrow herb into 1 glass of boiling water, steam for 1 hour. Drink 0.5 cups daily 2-3 times a day before meals.
Sage in the treatment of urinary incontinence with folk remedies
Pour 40 g of dry sage herb into 1 liter of boiling water, leave, covered, for 1-2 hours. Take 0.5-1 glass 3 times a day.
Folk remedy for urinary incontinence, treatment
Pour 3 tablespoons of shepherd's purse herb with 2 cups of boiling water, leave in a thermos for 3-4 hours. Drink 0.5 cups in 4 doses before meals.
Treatment of urinary incontinence with St. John's wort and centaury, a folk remedy
Mix equal parts of St. John's wort and centaury herb. Pour 1 teaspoon of the mixture into 1 glass of boiling water and leave. Drink 2 cups a day. The course of treatment is 2-3 weeks.
Folk remedy: St. John's wort and lingonberry for urinary incontinence, treatment
Mix 2 tablespoons of St. John's wort herb and 2 tablespoons of lingonberry leaves and berries. Pour the mixture with 3 cups of boiling water, boil for 10 minutes over low heat, cool, strain. Drink in small sips from 4 pm until bedtime.
Urinary incontinence: treatment with blackberries and blueberries, a folk remedy
Mix 1 tablespoon of blackberries and 1 tablespoon of blueberries, boil in 0.5 liters of water over low heat for 20 minutes. Leave, wrapped, for 30 minutes. Drink 1 glass 4 times a day.
 Pine cone jam is a cure for all diseases.
Pine cone jam is a cure for all diseases.
Urinary incontinence

Impaired urinary continence is a common, complex problem that significantly affects the quality of life of people experiencing it. Fortunately, the current availability of high-tech surgical treatments and effective medications at the disposal of specialist doctors means that treating urinary incontinence is challenging, but not impossible. The information that will be presented below will help you navigate the problem of urinary incontinence even before visiting a urologist.
What is urinary incontinence?
Urinary incontinence refers to any involuntary loss of urine. This is not a disease, but a symptom that can be caused by a wide variety of pathologies. Urinary incontinence can occur with diabetes, multiple sclerosis, after a stroke, injuries and operations on the spine, in women with prolapse and without vaginal walls, after childbirth and operations on the uterus, in men with an enlarged prostate gland and after operations on it for benign and malignant tumors. It is generally believed that urinary incontinence is a problem for older people. Indeed, in the general population over 65 years of age, urinary incontinence occurs in 25% of women and 15% of men. However, urinary incontinence is quite common among young, socially active women.
What are the main types of urinary incontinence?
Stress urinary incontinence - is the most common type of urinary incontinence. Uncontrolled loss of urine occurs when intra-abdominal pressure increases, which can be caused by completely ordinary events (walking, laughing, coughing, sneezing, etc.). The essence of the problem is the loss of support for the urethral sphincter, even with a slight prolapse of the vaginal walls - in young women. a decrease in sphincter tone and internal urethral resistance due to a decrease in estrogen levels - in menopausal women.
In men, the most common cause is previous prostate surgery, usually radical prostatectomy for cancer, rarely transurethral resection or adenomectomy for benign hyperplasia.
Urgent urinary incontinence - the second most common type of urinary incontinence. It is observed in patients with an overactive bladder. Urinary incontinence occurs immediately following an uncontrollable urge to urinate, while the patient is unable to suppress this urge in time to reach the toilet. Quite typical provoking factors are the sound of dripping water, waking up at night and changing body position, opening the doors of your own apartment with a key. Urinary incontinence most often occurs with neurogenic bladder overactivity (stroke, multiple sclerosis, spinal injury).
Diagnostics.
As with any diagnosis of urinary incontinence, a thorough medical history and a thorough physical examination are critical. Very important aspects in the patient survey are fluid intake and toilet habits, bowel function (constipation). When collecting anamnesis, attention is paid to heredity and previous surgical interventions on the pelvic organs. The initial assessment includes a urine test, a voiding diary, and a chairside examination to detect urine loss from coughing or straining (stress test). In cases of planned surgical intervention or an unclear clinical picture, a urodynamic study is mandatory. Complex urodynamic study (CUDI) - to date, the only method that allows you to reliably assess the functional state of the lower urinary tract. This test is performed on an outpatient basis, takes about 20-30 minutes and does not cause pain.
Treatment methods for urinary incontinence.
The choice of treatment method is based on an accurate diagnosis and depends on the type of urinary incontinence.
Stress urinary incontinence Non-invasive treatments for this type of urinary incontinence include exercises to train the muscles of the perineum (known as Kegel exercises). However, we must remember that the effectiveness of this method (improvement) is no more than 70%, given that the exercises must be performed continuously for at least 6 months. For quite a long time it was believed that in all cases of stress urinary incontinence it was necessary to start with exercises and only then consider the possibility of surgical treatment. In the last decade, attitudes to this issue have been revised, and surgery is now the first line of treatment in most cases. Anterior colporrhaphy (plasty of the anterior vaginal wall) 10-15 years ago was considered by gynecologists as the main operation for the treatment of women with stress urinary incontinence. However, an assessment of the long-term results of this operation showed that its effectiveness does not exceed 50%. Currently, most gynecologists do not consider it possible to offer this method of treating urinary incontinence. For a long time, the Burch operation (pulling the vaginal wall to the pubic bones using non-absorbable sutures) was considered the “gold standard” in the treatment of women with stress urinary incontinence. Compared to modern methods of surgical correction of urinary incontinence, this method is traumatic and requires more time for recovery. However, if laparoscopic surgery is performed for diseases of the internal genitalia (for example, uterine fibroids), it is advisable to perform a laparoscopic version of the Burch operation in a patient with concomitant urinary incontinence. Currently, there is no doubt that the main operation for the treatment of stress urinary incontinence in women is the implantation of a synthetic tape in the area of the middle part of the urethra (suburethral sling), installed from the retropubic or transobturator (through the obturator foramen) position.
In men with urinary incontinence after prostate surgery, an attractive method is the injection of so-called volume-forming drugs (gels) into the sphincter area. The injections are performed under local anesthesia and can be done multiple times. Unfortunately, the effectiveness of this treatment method ranges from 10% to 30%. In recent years, specialists have shown interest in male slings. It should be noted that the different pathophysiology of urinary incontinence and the anatomical features of the male urethra and pelvis do not allow obtaining decent results. The most effective method of surgical treatment of urinary incontinence in men remains implantation of an artificial sphincter. The device consists of a cuff that is placed around the urethra, a balloon and a pump (pump) that is placed under the skin of the scrotum for patient-controlled urination.
Urgent urinary incontinence - Treatment of this type of urinary incontinence consists of conservative measures and drug therapy. First of all, you need to try to change your usual life patterns (avoid eating spices, alcohol and coffee). In general, there are no restrictions on fluid intake, but it is not recommended to drink fluid in the evening and at night. As mentioned in the section on treating stress urinary incontinence, Kegel exercises are helpful, but the patient must be committed to this type of treatment. Based on the data from the urination diary, the patient should try to restore voluntary control over urination by gradually increasing the intervals between voiding. The main treatment for overactive bladder, accompanied by urge incontinence, is to take medications that relax the bladder (anticholinergics). Vesicare, driptan, detrusitol, and spasmex are registered and approved for use in our country. Recently, generics (drugs that contain the original drug molecule, but are produced by another pharmaceutical company) have begun to appear in pharmacies. The disadvantages of anticholinergic drugs include not so rare side effects, such as dry mouth, constipation, and blurred vision. Sometimes, even with good effectiveness, some patients refuse to continue treatment due to side effects. An achievement in recent years in the treatment of urge incontinence has been the use of intravesical injections of botulinum toxin. This is especially true in patients with drug-resistant and neurogenic bladder overactivity with urinary incontinence. Finally, there is a method of implanting special devices that allow you to modulate (change) the function of the bladder. Unfortunately, due to the high cost of equipment, this method has not yet received sufficient distribution in our country.
Overflow incontinence - in these cases, the fundamental question is to determine the cause of this type of urinary incontinence. If there is an obstruction to the outflow of urine (hyperplasia, stricture disease of the urethra, etc.), the task is to eliminate bladder outlet obstruction or urine diversion. If bladder contractility is impaired, the patient requires periodic catheterization (emptying the bladder) to minimize urine loss and preserve kidney function.
What can you expect from treatment?
The ultimate goal of any treatment is to improve the quality of life of patients. And believe me, in most cases this is possible. But the result largely depends on the patient himself. Drug therapy for overactive bladder will be effective if the patient does not drink 4-5 liters of fluid per day. The positive result of surgery for stress urinary incontinence will be long-term if the patient does not gain 30 kilograms in weight. That is, long-term positive treatment results directly depend on the common sense with which the patient approaches his health.
In general, the cure rate for women with stress urinary incontinence operated on using modern techniques is close to 92%. A stable bladder condition can be achieved in 75-80% of patients with urge urinary incontinence. The effectiveness of artificial sphincter implantation operations is 70-80%.
Epidemiology
Stroke is often accompanied by urological complications, the nature of which depends on the location and degree of brain damage due to cerebrovascular disease. One of these complications is urinary incontinence, which occurs in 25-44% of elderly people. It is believed that in the acute stage of stroke, urinary incontinence is observed in 50-70%, and this complication persists in the late period only in 15-30%. Moreover, they provide information that 51% of patients who have suffered a stroke have urinary incontinence in the first year, and only 15% continue to have it in the future. This may be due to a certain extent to the fact that urinary incontinence is not always a consequence of a stroke, because in 17% urinary incontinence is observed before it. A convincing meta-analysis of 2800 stroke survivors revealed urinary incontinence in the acute period upon admission in 32-79% of patients, and on the day of discharge it remained in 25%.
Borrie et al. Based on a survey of 151 patients in the acute stage of stroke, they noted a significant connection between urinary incontinence and the severity of motor disorders, mental disorders and decreased activity. Subsequently, it was shown that the severity of urinary incontinence is an independent factor in the prognosis of severe course and outcome of stroke.
There is evidence of a possible relationship between the risk of death, and within the first year, in patients with urinary incontinence after a stroke. For example, there is data that in this case the mortality rate in patients without urinary incontinence was only 7%, and in patients with urinary incontinence it reached 52%. This dependence of the probability of death after a stroke complicated by urinary incontinence has been studied and confirmed by many studies, as well as the development of disability after 3 and 12 months. with a specificity of 78%. In addition, difficult care of such patients was a more common reason for their transfer to hospice than the presence of aphasia and even mental disorders. It is important to note that urinary incontinence is often an independent cause of hospitalization.
Pathogenesis
Normally, urination and urinary retention are controlled by a reflex arc running from the bladder to the pons and then by control of the cortex, which interacts with the motor centers and suprasacral pathways of the spinal cord. The pathophysiology of urinary incontinence after stroke is based on three mechanisms:
damage to the conduction tract and urination centers,
motor and mental disorders,
paradoxical ischuria without a direct connection with stroke.
On this basis, one can explain the transient nature of urinary disorders after a stroke as motor and mental functions are restored - one can expect, and this happens, the ability to retain urine is restored. On the other hand, incontinence, which is not directly related to neurourological causes, may be the result of a stroke with damage to the frontal lobe, in which the patient does not pay attention to the need to urinate. In the case of neurological causes of urinary incontinence, its nature is determined by the location of the stroke, the severity and extent of brain damage and the functional role of its area. Attempts to localize the areas of the brain directly responsible for the regulation of urination in normal conditions and when they are damaged continue to this day. It has become known that detrusor overactivity is a consequence of interruption of the suprapontine pathways, which normally have an inhibitory effect through the efferent pathways of the spinal cord. It was possible to show that the areas of the brain that control the functions of storage and emptying of the bladder are located in the superomedial part of the frontal lobe and genu of the corpus callosum, which are connected through the basal ganglia to the reticular formation of the bridge. Moreover, it was possible to establish that damage to the right hemisphere leads to the occurrence of urge urinary incontinence, and with damage to the frontoparietal lobes and internal capsule, patients suffered not only from detrusor overactivity, but also from impaired control over the function of the urethral sphincter. Damage to the frontotemporal region caused involuntary contractions of the bladder with urge urinary incontinence in patients. On the other hand, when the cortex and internal capsule were not affected, patients maintained control of the urethral sphincter.
Thus, the neurourological consequences of stroke, in terms of urodynamic disorders, depend on the area of the brain affected. An acute disruption of conduction between the centers of the central nervous system that regulate urination and the nerve pathways themselves can lead to detrusor areflexia. In this case, the bladder is not able to contract; the normal tone of the urethral sphincter allows urine to be retained until paradoxical ischuria develops, which occurs in 21% of patients. Detrusor areflexia is usually observed in the acute period of stroke, and upon transition to the stable stage of stroke it disappears in most patients. On average, acute urinary retention occurs in the first 4 weeks of stroke in every third patient, and this is associated with mental disorders, diabetes, and urinary tract infections. Of these, 96% of patients urinate independently by the time of discharge. After an acute period of stroke (“brain shock”), the most common complication is detrusor overactivity with normal urethral sphincter function. Detrusor-sphincter dyssynergia (DSD) is observed after a stroke only in patients with additional or existing spinal cord lesions. Uncoordinated contractions of the urethral sphincter after a stroke in some patients are mistaken for DSD, since this is pseudodyssynergia, which is a manifestation of conscious or subconscious attempts of patients to prevent urinary incontinence by contracting the urethral sphincter during involuntary contractions of the detrusor. Some authors observed detrusor hyperactivity after a stroke in 46%, others even in 100% after a brain injury, but DSD was not established in any of these patients.
Urological complications during different periods of stroke and their management
It is important to treat urological complications in accordance with the clarification of the pathophysiology of their occurrence and development during and post-stroke periods, which is based on anamnesis data, especially in the pre-stroke period, because the identified data can often greatly help in treatment tactics to restore or improve urination. For example, an overactive bladder, residual urine manifested as lower urinary tract symptoms (LUTS) can be caused by diseases of a “purely” urological nature.
Acute period (phase) of stroke. This period lasts from several days to several weeks, followed by a transition to a recovery period of varying lengths and ends with a period of stabilization.
Immediately after the development of a stroke, the doctor, paying attention to the urological status and identifying acute urinary retention, resorts to a permanent catheter or intermittent catheterization. In dynamics, further events develop according to the following options: restoration of urination without or with residual urine, chronic urinary retention, urinary incontinence. It is necessary to determine residual urine, moreover, using an ultrasound method, which can be used in the dynamics of observation without the risk of infection, which may be a consequence of catheterization.
Other complications of the acute period of stroke may include:
paradoxical ischuria,
lower urinary tract infections,
detrusor overactivity.
If the first is managed by catheterization, the second by antibacterial drugs in accordance with the results of urine culture, then an overactive detrusor, and in this case we can talk about neurogenic overactive bladder (OAB), makes long-term treatment necessary. In this case, it is important to know that the patient has urological diseases such as prostate hyperplasia, which can be an independent cause of detrusor overactivity. Do not forget about possible vertebrogenic lesions (herniated disc, etc.). In these cases, a-adrenergic blockers (tamsulosin, alfuzosin, doxazosin) and/or anticholinergic drugs (trospium chloride, tolterodine tartrate, solifenacin) are used, and trospium chloride, due to its pharmacological characteristics, is more indicated for patients after a stroke, especially the elderly.
After a stroke, many patients also experience other LUTS, especially those that are a consequence of catheterization - dysuria, and sometimes even terminal hematuria, the occurrence and duration of which may be a consequence of disease of the prostate and female genital organs.
In addition to treating these complications of catheterization with antibacterial and other anti-inflammatory drugs, it is important to remember the need to prevent infection during catheterization: sterility in this case (gloves, gown, treatment of the external genitalia, the need to assist the doctor) is a predictor of success.
The recovery period is characterized by the duration of the dynamics of improvement in the neurological condition: it can last from several days to several years, but most often about a year. At this time, symptomatic therapy and urodynamic studies are recommended. The changes found in this case make it possible to clarify the possibilities of pathogenetic therapy.
The most common symptom observed in the patient is detrusor overactivity, sometimes with residual urine. In this case, the experience of a urologist and the timely attention of a neurologist allow you to choose a set of measures. For example, with a large amount of residual urine (500 ml or more), autocatheterization can be used in women, and a permanent catheter in men. In the latter case, it is advisable in old age, especially in the presence of prostate hyperplasia, to perform bilateral ligation of the ductus deferens to prevent acute epididymitis. During this period of stroke, treatment with anticholinergic drugs is, of course, continued.
Sphincteric urinary incontinence is usually a consequence of diseases before a stroke and is observed extremely rarely. The cause of such incontinence is often disorders of the pudendal nerve, congenital or acquired. If such a complication of an acquired disease, you can try to use electrical stimulation of the tibial nerve. Palliative treatment involves urinating by the hour, limiting fluid intake, pads or an indwelling catheter with periodic clamping, for no more than 3-4 hours.
In case of urinary retention due to impaired detrusor tone (areflexia), preference is given to intermittent catheterization. In case of bladder outlet obstruction due to prostatic hyperplasia, its dynamic component is removed by prescribing a-blockers, often in combination with tadenan, prostamol uno, in the hope of their powerful anti-edematous effect, as experience has shown us. A permanent catheter is used if the above recommendations have no effect or are inconvenient.
The stable stage, which is considered to be the time when there is no improvement in neurological status, usually occurs 1-2 years after the stroke (Fig. 3). The most common urological complication of this period is urinary incontinence. It is believed that in this case, the treatment of urinary incontinence can be treated similarly to the treatment of patients without cerebrovascular disease. Thus, urge urinary incontinence is usually part of the clinical course of OAB. In this case, the urgency can be treated with the anticholinergic drugs given earlier, as well as capsaicin, resiniferatoxin, or botulinum toxin in the detrusor and electrical stimulation of the tibial nerve. If by the time of the stable stage there are urinary disorders in the form of urinary retention, sacral neuromodulation can be performed, which in recent years has been successfully used for symptoms of neurogenic bladder.
Conclusion
Thus, urological complications can be considered common in patients after a stroke. The frequency and severity of these complications depend on the area of the brain affected and its size. After examining such patients by a neurologist, at the same time they should be consulted by a urologist. In the future, patients are observed by a urologist systematically for timely prescription or replacement of prescribed medications and other types of treatment. Impaired quality of life in patients who have suffered a stroke depends on both neurological and no less severe urological consequences. Timely treatment of the latter at all stages of the post-stroke period is the urologist’s contribution to the rehabilitation and return to the family of these patients, where their care will be significantly easier.
The article was published in the journal "Medical Estate" 2007, No. 2, p. 15-18
Literature
1. Peet SM, Castleden CM, McGrother CW. Prevalence of urinary and faecal incontinence in hospitals and residential and nursing homes for older people. BMI 1995; 311:1063–1064.
2. Tobin GW, Brocklehurst JC. The management of urinary incontinence in local authority residential homes for the elderly. Age Aging 1986; 14:292–298.
3. Palmer MH, German PS, Ouslander JG. Risk factors for urinary incontinence one year after nursing home admission. Residential Nursing Health 1991; 13:405–412.
4. Redding MJ, Winter SW, Hochrein SA, et al. Urinary incontinence after unilateral hemispheric stroke: a neurologic epidemiologic perspective. J Neurorehab 1987; 1:25.
5. Brocklehurst JC, Andrews K, Richards B, Laycock PJ. Incidence and correlates of incontinence in stroke patients. J Am Geriatric Soc 1985; 33:540–542.
6. Brittain KR, Peet SM, Potter JF, Castleden CM. Prevalence and management of urinary incontinence in stroke survivors. Age and Aging 1999; 28:509–511.
7. Borrie MJ, Campbell AJ, Caradoc–Davies TH, Spears GFS. Urinary incontinence after stroke: a prospective study. Age and Aging 1986; 15:177–181.
8. Anderson CS, Jamrozik KD, Broadhurst RI, et al. Predicting survival for / 1 year among different subtypes of stroke. Stroke 1994; 25:1935–1944.
9. Nakayama H, Jorgenson HS, Pedersen PM, et al. Prevalence and risk factors of incontinence after stroke: the Copenhagen stroke study. Stroke 1997; 28:58–62.
10. Matthews WB, Oxybury JM. Prognostic factors in stroke. In: Ciba Foundation Symposium, No. 34. Amsterdam: Elsevier, 1975:1–279.
11. Jimenez J, Morgan PG. Predicting improvement in stroke patients referred for inpatient rehabilitation. CanMed Assoc J 1979; 121:1481–1484.
12. Wade DT, Hewer RL. Outlook after acute stroke: urinary incontinence and loss of consciousness compared in 532 patients. Quart J Med 1985; 56:601–608.
13. Taub NA, Wolfe CD, Richardson E, et al. Predicting the disability of first–time stroke sufferers at 1 year. 12 month follow-up of a population-based cohort in Southeast England. Stroke 1994; 25:352–357.
14. van Kuijik AA, van der Linde H, van Limbeek J. Urinary incontinence in stroke patients after admission to a postacute inpatient rehabilitation program. Arch Phys Med Rehabil 2001; 82:1407–1411.
15. Ouslander JG, Kane RL, Abrass IB. Urinary incontinence in elderly nursing home patients. JAMA 1982; 248:1194–1198.
16. Noekler LS. Incontinence in elderly cared for by family. Gerontologist 1987; 27:194–200.
17. Gelber AG, Good DC, Laven LJ, Verhulst SJ. Causes of urinary incontinence after stroke: a prospective study. Age Aging 1986; 15:177–181.
18. Blaivas IG. The neurophysiology of micturition: a clinical study of 550 patients. J Urol 1982; 127:958–963.
19. BradleyWE, Timm GW, Scott FB. Innervation of the detrusor muscle and urethra. Urol Clin NAm 1974; 1:3.
20. Chancellor MB, YoshimuraN. Physiology and pharmacology of the bladder and urethra. In: Walsh PC, ed. Campbell's urology, 8th edn. Philadelphia: WB Saunders, 2002:813–886.
21. Gosling J. Anatomy (physical and neural) of the lower urinary tract. In: Schick E, Corcos J, eds. Neurogenic bladder, adults and children. New York: Marcel Dekker, 2003.
22. Kuroiwa Y, Tohgi H, Ono S, Itoh M. Frequency and urgency of micturition in hemiplegic patients: relationship to hemisphere laterality of lesions. J Neurol 1987; 234:100–102.
23. Burney TL, Senapati M, Desai S, Choudhary ST, Badlani GH. Effects of cerebrovascular accident on micturition. Urol Clin North Am 1996; 23(3):483–490.
24. Khan Z, Starer P, Yang WC, Bhola A. Analysis of voiding disorders in patients with cerebrovascular accidents. Urology 1990; 35:265–270.
25. Kong KH, Young S. Incidence and outcome of poststroke urinary retention: a prospective study Arch Phys Med Rehabil 2000; 81(1):136–143.
26. Wein AJ, Barrett DM. Etiologic possibilities for increased pelvic floor electromyographic activity during cystometry. J Urol 1982; 127:949–952.
27. Staskin DS, Vandi Y, Siroky, MB. Postprostatectomy incontinence in the Parsonian patient: the significance of poor voluntary sphincter control. J Urol 1988; 140(1): 117–118.
28. Badlani GH, Vohra S, Motola JA. Detrusor behavior in patients with dominant hemispheric strokes. Neurourol Urodynam 1991; 10:119–123.
29. Krimchansky BZ, Sazbon L, Heller L, et al. Bladder tone in patients in post–traumatic vegetative state. Brain Inj 1999; 12(11):899–903.
30. Flisser AJ, Blaivas JG. Cerebrovascular accidents, intracranial tumors and urologic consistency. Textbook of Neurogenic Bladder. Ed. by J. Corcos, E. Schik. MD Taylor & Francis group, London & New York, 2004
31. Chartier–Kastler EJ, Bosch JLHR, Perrigot M, et al. Long–term results of sacral nerve stimulation (S3) for the treatment of neurogenic refractory urge incontinence related to detrusor hyperreflexia. Urol 2000; 164:1476.
32. Jonas U, Grunewald V, eds. New perspectives in sacral nerve stimulation. London: Martin Dunitz, 2002.
Urinary incontinence after a stroke is very common, as are problems with bowel movements. As you know, a stroke is a very dangerous pathology that can cause death. But if you receive timely medical care, it is still possible to save the patient’s life, although often the consequences of a stroke are very serious. The person has to relearn normal things like walking and talking, as well as cope with some changes in the body.
Urinary and fecal incontinence after a stroke is a huge nuisance, which you can still get rid of. Treatment of such pathologies is one of the important activities that are carried out in relation to people who have suffered a stroke. Many people believe that if they have such a symptom, they will never be able to lead a normal life.
But in fact, there is no need to despair, since it is still possible to get rid of the trouble, although it can be very difficult to eliminate the consequences of a stroke. The patient must gain strength and patience, because rehabilitation after such a serious test of the body will be long.
Causes of incontinence
The consequences of a stroke can be different. Fecal and urinary incontinence are one of the common troubles associated with this disease. Most often, it is precisely because of the inability to contain waste fluids in the body that patients have to spend a lot of time in the hospital after a stroke.
However, it must be borne in mind that such a complication is not incurable. It is possible to get rid of incontinence, but for this the patient must carefully adhere to the doctor’s recommendations and make an effort in the fight against this pathology. Only with a strong desire for a complete cure can we say that the patient will be able to overcome his illness and return to normal life again.
Urinary and fecal incontinence occurs very often immediately after a stroke. However, in most patients, this pathology completely disappears within a week. Among those whose incontinence does not disappear completely, there are patients who note a significant decrease in the manifestations of this symptom.
Still, the inability to keep fluids in the body is a fairly common problem. There is no need to remain silent about her. If a person is concerned about such a symptom, he should definitely inform his doctor about it. Otherwise, there will be nowhere to wait for help.
The specialist must conduct a thorough diagnosis, and then tell the patient how to properly deal with the problem.
Among the complications of stroke, enuresis is much more common than the inability to hold feces. The frontal lobe of the brain is responsible for this process. However, if the disease damages this section, then over time the spinal cord begins to control the bladder. The task of the doctor and the patient will be to work hard to ensure that the transfer of functions is successful and the body begins to function normally again.
In most cases, with careful therapy, incontinence is eliminated within a month. If this does not happen, a more in-depth examination is carried out in order to identify the cause of what is happening. Once the diagnosis is made, the doctor can prescribe the most appropriate treatment. Often, this requires examination by specialized specialists, including a urologist.
Additional diagnostics may show the presence of infections in the bladder or urinary tract. This is a fairly common reason why incontinence after a stroke does not go away for more than a month. Treatment is carried out with powerful antibiotics. Proper drug therapy allows you to forget about the problem completely.
Incontinence can also be caused by medications that are intended to eliminate some of the consequences associated with a stroke. In this case, it is important to review the list of medications, and then exclude the use of those that negatively affect the genitourinary system.
Instead, the doctor may prescribe medications that will help control urination. Such drugs are especially useful when taken in the evening, as they can reduce the flow of fluid into the bladder at night.
Treatment without drugs
For problems with urinary incontinence after a stroke, medications are often prescribed. However, it is important not only to stop the unpleasant symptom, but also to teach the body to fight it. Otherwise, the pathology will return again and again, and the patient will have to constantly take pills.
To prevent such developments, you need to train your body. First you need to train yourself to go to the toilet at the same time. This way the body will get used to the schedule, and involuntary urination will disappear. You can set a reminder on your phone so you know exactly when you need to go to the restroom. In addition, you need to be prepared for the fact that you will have to wake up often at night. However, this is a temporary phenomenon. With proper treatment, the problem will gradually disappear.
It is necessary to train your body after a stroke. This is important, because otherwise no drug therapy will help. If you follow all the rules of rehabilitation and follow the doctor’s recommendations, you can achieve good results.
While the problem of incontinence continues to bother the patient, it is necessary to use diapers and absorbent waterproof diapers. This will avoid awkward situations. All hygiene products must be changed promptly. This is very important, since urine and feces contain a large number of harmful bacteria; if their concentration in the genital area is too high, this can cause an infectious disease. In this case, treatment for urinary incontinence will not take long.
Can incontinence be treated with pills?
The problem of the inability to retain fluid in the body after a stroke occurs in almost 80% of people who have suffered a similar illness. But after a week in most patients the symptom disappears on its own. The rest have to deal with the problem using special methods.
It is worth noting that the fair sex is much less fortunate in this regard. Women with incontinence after a stroke are more common, but this does not mean that this complication is easier to treat in men.
In medical practice, medications are used that can temporarily eliminate uncontrolled urine output. But they are not able to completely cure the problem. The complication of urinary incontinence after a stroke can only be eliminated by training your body, and for this you will have to do a lot of work on your body.
Medicines will be useful only in cases where the cause of the inability to retain fluid is an infection. In such a situation, the doctor prescribes antibacterial therapy, which speeds up the disappearance of such a nuisance as incontinence.
How to deal with fecal incontinence?
Problems with involuntary urination in men and women who have suffered a stroke occur much more often than problems associated with feces. However, a considerable percentage of victims still encounter a similar complication. About a third of patients experience problems with fecal incontinence in the first week after a stroke. But most manage to regain control of their intestines fairly quickly.

Those patients who have suffered a stroke with obvious dementia are more susceptible to the problem of fecal incontinence. In this case, you will have to carefully select the food for the patient so that the food does not cause either constipation or diarrhea. Fiber should be included in the daily diet if a person has no problems swallowing food. In addition, you need to monitor the body's water balance. It is important to avoid dehydration at all costs. The norm is 30-40 grams of pure water or tea without sugar per 1 kilogram of weight.
However, this moment is individual. If the patient has a problem such as urinary incontinence, plus heart pathology, the amount of fluid should be significantly less. It is advisable to discuss this issue with your doctor. In addition, the doctor must create the most suitable diet that will allow you to survive this difficult period with minimal discomfort. With the right approach, a person, even after a complex stroke, will be able to take control of his bladder and intestines.
Particular attention should be paid to physiotherapy and muscle training. They play a very important role in recovery after a stroke. It is necessary to follow all the doctor’s recommendations correctly and avoid overload. Training beyond one's own strength can result in new complications.
Stroke Prevention
In order not to face such a problem as a stroke, a person should monitor his health at any age. Recently, the problem is increasingly affecting the younger generation. The reason for this is poor nutrition, bad habits and a sedentary lifestyle. In addition, you need to be careful about medications. Using some medications without a doctor's recommendation can cause side effects, including bleeding.
If such a disaster occurs, you need to immediately take the patient to a doctor. Only timely medical assistance gives a chance of life to a person who has suffered a stroke.
2015-05-02 14:55:56
Marina asks:
Hello! My father has been in bed for 5 years after a stroke. Now a new sore has appeared. Sores appeared on the head of the penis (more than a month ago. He has incontinence, he has never used diapers, there is a urine collector. I thought it was the urine that was corroding, a rash appeared between the legs. The urologist recommended zinc ointment, the dermatologist flucanozol 100, 1 capsule, Deloskin powder, lotions, amoxil sprinkled with methyluracil 3 times per tablet. The rash has gone away. The wounds remain and have increased, not only on the head but on the penis itself the skin is peeling off (it turns white and peels off), swelling has appeared. What should I do?
Answers Mazaeva Yulia Alexandrovna:
Hello, if urinary incontinence causes severe damage to the skin and mucous membranes due to the aggressive effects of urine, it is recommended to install a permanent urethral catheter.
2010-12-05 13:41:45
Yuri asks:
Hello, doctor! On April 6, my mother (65 years old) suffered an ischemic stroke of the right temporal hemisphere of the brain. They immediately called an ambulance - they did something for my blood pressure and a cardiogram. The last days before this, the mother had high blood pressure (approximately 220/100). On the day of the stroke, my mother fell and could not get up, and then the stroke happened... She lives in my village alone. She managed to take a cell phone and call a neighbor. SHE CALLED AN AMBULANCE. She was taken to the regional hospital in Ardatov, Mordovia. It was difficult to admit her to the hospital due to a lack of beds. There was no doctor, he had a day off!??? One of the service staff was a nurse. She couldn’t help but do anything. We lay there for a day without any help. Me, her son and sister arrived immediately 300 km from the hospital. When the doctor came for lunch, we immediately asked him to give a referral to the regional hospital. We got it with difficulty. The regional republican hospital is 120 km away. When we got there, she was still moving on her own. We went up to the 3rd floor and the doctor examined her. Her leg and arm were still working. They admitted us and began intensive treatment.
Here is the research protocol:
“In the right frontal parietal part on the right, a large, about 37 * 37 * 92 mm area of density, heterogeneous is visible. The ventricles are not examined, the lateral walls of the membrane, near-edema! Signs of hypertension are visible (sorry for the inaccuracy, it is not clearly written). The cut structures are not displaced .
Conclusion: infarction in the right hemisphere of the brain.
Extract from medical history
The patient was in the neurological department from 04/09/10 to 04/30/10 with the diagnosis: Ischemic stroke from 04/08/10. Atherothrombotic cerebral infarction in the right MCA basin, progressive course. Left-sided hepiplegia. DE (mixed origin) 2nd stage.
Objectively: BP150/90 mmHg. Heart rate 80/min.
ST NEVR Consciousness preserved.
Palpebral fissures, pupils D=S/Smoothed left i/g fold. Left-sided superior monoparesis. Limb reflexes. D During her stay in the hospital, the patient’s condition worsened, left-sided hemiplegia appeared.
Examination: UAC dated 04/10/10 L-6.5 10; Hb 124g/l; ESR 40mm/hour;e 1; p/box 2, s/box 68; monocytes 8; lymphocytes 23; blood sugar 7.3 mmol/l
Biochemical blood test dated 04/10/10 Total protein 71, Urea 4.4; Creatinine 58; cholesterol 6.7, AST 27; ALT 30;
OAM from 04/10/10 l2-3 in p/zr, ep 3-5, beat. weight 1023, neutral
Oculist 04/12/10. Retinal angiopathy (hypertensive).
CT scan of the brain from 04/15/10 Infarction of the right hemisphere of the brain.
Examination by a psychiatrist dated 04/16/10 Psychoorganic damage to the central nervous system with hallucinatory syndrome.
ECG from 04/09/10 Sinus rhythm 75 per minute. Normal position of the EOS. Slowing of AV conduction. Dystrophic changes in the myocardium of the left ventricle.
Treatment: enalapril, pentoxifylline, riboxin, nicotinic acid, VitV, Cavinton, Actovegin, Mexidol, beckons, gliatelin, massage, exercise therapy, session with a rehabilitation specialist.
Recommended:
1) D-observ. neurologist
2) Cortexin 10 mg IM No. 10
3) Cavinton 2 tablets. 3 times a day
4) Passing the ITU
5) Plavix 75 mg. 1 time a day constantly
doctor, 8 months have passed since the stroke, at the moment we have changed our place of residence. I took my mother to my place in Ulyanovsk. Mom still can’t walk, but that’s not all, at first she seemed to be getting better. Then, at 6 months, I asked my local doctor for a course of cerebralysin solution, Cavinton 2 mg-5 pcs., Actovegin 5 mg-5 pcs. Two weeks passed after the instillation, but the condition did not improve, but rather worsened. Now her legs are like cotton wool, she can’t straighten up on them, although we used to move with my help. There is urinary incontinence. We take lozap tablets 25 mg 1 tab. in the evening, indapamide 1 tablet in the morning, zilt. Pressure 126-86 is normal and during physical activity 144-111.
QUESTION: Why does this happen? After all, we were moving towards improvement, albeit slowly, but improvement. A neurologist arrived once in an ambulance and quickly looked and asked what complaints he had. I wrote down the diagnosis and left. Should I take Cavinton or something else? I'm afraid it will be even worse.
Answers Kachanova Victoria Gennadievna:
Popular articles on the topic: urinary incontinence after stroke
In recent years, the number of cerebral strokes (MI) has been progressively increasing throughout the world, primarily due to ischemic disorders of cerebral circulation. In the coming decades, WHO experts expect a further increase in the number of ischemic...
In continuation of the coverage of the master class held as part of the conference “Hormones and Women’s Reproductive Health,” we present to the readers a lecture by the head of the department of the Scientific Center for Obstetrics, Gynecology and Perinatology, Professor E.V. Uvarova