Premature aging placenta - a threatening condition. Any pregnant woman can encounter it. Why does the “children’s place” begin to lose its functions? ahead of schedule and what to do with these, we will tell you in this article.
How does the “children's place” mature?
The “baby place”, or placenta, is a temporary organ necessary for a woman and child only during pregnancy. It has a spongy structure, one side fits tightly to the wall of the uterus, from where it draws reserves of maternal blood, and the other is connected to the fetus through the umbilical cord. The placenta performs protective functions, preventing the blood of mother and baby from mixing. It also acts as an intermediary in gas exchange and nutrition: through the placenta, through a vein in the umbilical cord structure, the baby receives fresh blood with oxygen and vitamins, and through two arteries inside the umbilical cord, waste products of the baby are returned to the placenta: urea, carbon dioxide, creatinine. The placenta produces important for pregnancy and subsequent breastfeeding hormones.
A week after ovulation, the fertilized egg enters the uterine cavity and its main task is to implant. The chorionic membrane, which “grows” into the maternal endometrium, helps with this. At the site of attachment, a chorion is formed, which gradually transforms into the placenta. Formation " children's place“Completes by 14–16 weeks of pregnancy. The young placenta takes its final shape by 20 weeks. Until the middle of pregnancy, the “baby place” grows and expands. After this, it only slightly increases in thickness.

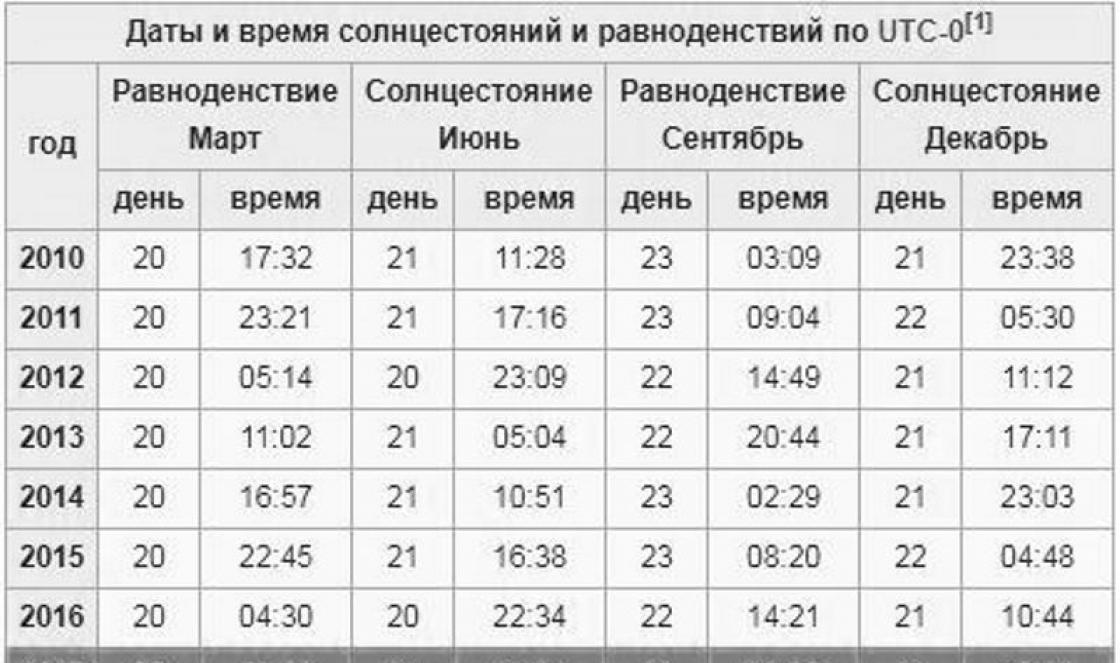
The closer to childbirth, the less functional the placenta is: it exhausts its resources and begins to age. First, its shells become wavy, then inclusions of calcium salt deposits appear in the placenta, then these inclusions become more extensive - the placenta changes from spongy to denser and begins to become thinner. All these processes fit into four degrees of maturity.
If the degrees succeed each other within the prescribed time limits, this does not pose any danger. If the placenta “fades away” too quickly, they talk about its premature aging.

Norms and deviations
Young and full of strength the placenta has zero degree of maturity. This means that the resources of the “children’s place” are not exhausted - the baby receives everything necessary for his development. Normally, zero degree of maturity is recorded before the 30th week of pregnancy.
The first degree of maturity of the placenta indicates that changes have begun: the growth of the network of vessels and tissues has stopped, the membrane becomes wavy. But the “children’s seat” performs its functions properly – the baby is comfortable, and there is enough of everything. The first degree normally corresponds to 30-34 weeks of pregnancy.
The second degree of maturity describes active regressive processes in the “baby place”: fragmentary thinning of the placenta may appear, its structure becomes more dense, and calcium salt deposits appear. If stage 2 is established within the normal time frame, you don’t have to worry - the placenta copes with its tasks without harming the baby. The second degree will not be considered pathological if the pregnancy is already 35–38 weeks.
Third degree - mature or old placenta. The structure, which previously resembled a fairly smooth cake, becomes lobed: lobes are defined, the membrane is uneven, salt deposits are clearly visible. Typically, stage 3 is recorded immediately before birth: in the last couple of weeks, and sometimes just a few days before birth.

If the doctor sets an intermediate degree, for example, 0–1 or 1–2, it means that the ultrasound showed signs of a transition from one stage of development of the “children’s place” to another, but the transition itself has not yet been completed. With transitional degrees, the most incomprehensible moments and misunderstandings usually arise. To make it easier to understand what is normal and what is not, you should know that grade 0–1 at 27–28 weeks of pregnancy is not a pathology, but a variant of the norm.
After 30 weeks, the doctor can diagnose both the first and transitional (0–1) degrees. But grade 1–2 at 32 weeks is an obvious pathology, since there is still about a month before the transition to the second degree. The onset of stage 3 maturity before 38 weeks is also an alarming and dangerous situation, in which, most likely, a decision will be made about early delivery.
The greater the time gap between the norm and the actual state of the placenta, the more dangerous the consequences can be.

Why is it dangerous?
Since nature entrusts the placenta with important functions of protection, nutrition, oxygen supply, as well as hormonal support for the pregnant woman’s body, any changes in the structure of the placenta ahead of time can lead to serious complications. When aging occurs on time, it is physiological: the loss of some functions of the placenta, their decrease, is compensated by the organisms of the mother and fetus. This does not harm the child, since normally the decline of the function proceeds quite smoothly.
If early maturation is observed, then the baby does not receive enough oxygen, the placenta copes worse with the removal of its waste products, and it lacks nutrients. In addition, the placenta copes worse with its protective functions. The most common consequence of premature maturation for a child is hypoxia.
Due to oxygen deficiency, the baby’s brain and nervous system suffer. Prolonged hypoxia can lead to the death of a child in utero. Often it is intrauterine hypoxia that causes developmental delays in the fetus and severe disturbances in the activity of the central nervous system.


Children who suffered from hypoxia in the womb are more painful, they may experience various neurological abnormalities, as well as dysfunction of the musculoskeletal system. In addition, such children learn worse, and disability is possible.
Lack of nutrients leads to delayed intrauterine development of the baby. It is diagnosed during pregnancy. The height, weight, and length of the fetal limbs lag behind the normal values characteristic for a specific period of pregnancy. Often, delayed physical development is accompanied by brain disorders and metabolic disorders, which after birth are defined as delays in mental and mental development. Various defects can develop against the background of fasting internal organs And skeletal system baby.
The slow removal of fetal waste products by an early ripened placenta creates a threat of intoxication and death of the child. And a decrease in the barrier functions of the “children’s place” can lead to infection of the baby with dangerous viruses, which can easily penetrate the bloodstream to the baby. Intrauterine infection is a condition that is regarded as a threat to the life of the child.

What is the reason?
The placenta matures ahead of schedule for a variety of reasons. Most often, doctors are faced with the phenomenon of premature aging of the placenta in women who continue to smoke while carrying a baby or cannot deny themselves the pleasure of drinking alcoholic beverages. In women who flatter themselves with the hope that “light” cigarettes are harmless and red wine is beneficial, this pathology occurs quite often after the 30th week of pregnancy.
However, the lack bad habits during and before pregnancy does not guarantee that problems with the placenta will not arise. The ripening of the “children's place” ahead of time can be a consequence of a viral infectious disease, for example, ARVI or influenza in the early stages, as well as sexually transmitted infections.
For pregnant women with Rh-negative blood, provided that they are carrying a baby with positive Rh factor, a Rh conflict may develop, in which the placenta begins to suffer almost at the stage of formation. Its early maturation is often a consequence of those immune processes that occur during a conflict in the body expectant mother.



If a woman had diabetes mellitus before pregnancy or she acquired gestational diabetes while pregnant, the likelihood that the placenta will quickly age is much higher.
With such ailments, placental hyperplasia (an increase in its thickness) is usually observed, which almost always leads to an early loss of its functions. Early aging of the “baby place” also occurs in women who have had several abortions: the thinned endometrium in this case cannot ensure the normal development of the placenta. In this case, it is thinner initially and ages much faster.
Chronic diseases of the expectant mother, especially if they concern the kidneys, liver, thyroid gland, heart and blood vessels, as well as blood clotting disorders increase the likelihood of premature maturation of the “baby place”.
Many medications can negatively affect the rate of placental maturation, which is why expectant mothers are strongly advised not to take any medications unless approved by their doctor. Contact of the expectant mother with toxic substances, varnishes and paints, solvents, bleaches and other chemicals also has a destructive effect on placental tissues and blood vessels. Working in a dangerous and hazardous industry increases the likelihood of negative changes in the rate of placental maturation.

Premature aging of the placenta is more often observed in women who live in large cities with unfavorable environmental conditions than in women who live in a village or small town where there are no large city-forming industrial enterprises. And also the pathology, according to the observations of doctors, is inherited - from mother to daughter.
Preeclampsia (late toxicosis) quite often leads to the aging of the “baby place” ahead of schedule. Dangerous from the point of view of the likelihood of developing a pathological condition are changes in blood pressure in the expectant mother and hypertension. If a pregnant woman has experienced even minor placental abruption at any stage of pregnancy or has a previa baby, the risk of early maturation is several times higher than in women who do not have such problems during pregnancy.


During pregnancy with twins or triplets, the risk of early maturation is higher than with a singleton pregnancy. And women with hormonal problems almost always experience placental abnormalities to one degree or another, including old placenta at inappropriate gestational ages.
Symptoms and signs, diagnosis
There is no way to feel the degree of maturity of the placenta, as well as determine its thickness and other parameters on your own. Accelerated maturation of the “children’s place” occurs completely without symptoms. That is why it is important to regularly visit a doctor, undergo all scheduled examinations, take tests and have an ultrasound scan. The sooner the anomaly is detected, the more favorable doctors' prognoses for future treatment will be.
Signs of premature aging of the placenta for more than later, when the consequences of fetoplacental insufficiency already appear, they are mainly felt as a change in the baby’s motor activity. ABOUT initial stage Hypoxia is indicated by increased activity: the baby’s movements become abrupt and can cause severe pain to the pregnant woman. So the baby tries to massage the placenta with its arms and legs, trying to get more oxygen.


Prolonged hypoxia manifests itself with the opposite signs - the baby almost stops moving. It goes into oxygen and nutrient saving mode, trying to expend as little energy as possible. A complete cessation of movements may be a sign of the baby’s death.
Only a doctor can establish the fact of hypoxia, intrauterine growth retardation, intoxication and other unfavorable conditions. This is why it is so important not to miss visits to the antenatal clinic.
If the baby’s behavior changes, the woman is prescribed a study of the placenta and the characteristics of the uteroplacental blood flow using DG, ultrasound, and CTG is also performed. Cardiotocography, which can be performed from 28-29 weeks of pregnancy, can give a fairly accurate answer to the question of whether the baby has changes in the condition.
The degree of maturity of the placenta is determined by ultrasound, starting from the 20th week of pregnancy. At earlier stages, neither the thickness of the “child’s place” nor its characteristics of maturity have diagnostic significance.


Treatment
Despite the fact that the consequences can be quite serious, a woman should not panic: premature aging of the placenta is always more favorable than its pathological immaturity. At early detection pathologies, doctors can help the baby and his mother. Treatment is usually carried out in a hospital setting.
The choice of action tactics depends on the timing. If premature maturation of the placenta is detected at 31-35 weeks of pregnancy, then doctors try to do everything possible to preserve and prolong it, because the baby at this stage is not yet ready to be born. The woman is monitored in the hospital, provided with the necessary therapy, and CTG is performed daily to find out whether the baby’s condition and well-being have changed. An ultrasound is performed every few days to monitor the processes occurring in the placental structures.
If the gestation period is more than 36 weeks, then with a high degree of probability doctors will decide on early delivery: induction of labor or a cesarean section. Although, if the degree of deviation from the norm is small, they can put it on hold and try to support the baby inside the mother’s womb with medication for at least two more weeks so that he has time to gain weight.

The standard treatment regimen contains antispasmodic drugs (“Papavern”, “No-shpa”) to reduce contractility smooth muscles of the uterus. To improve blood flow in the “mother-placenta-fetus” system, “Curantil” and “Actovegin” are used both in tablets and in the form of intravenous drips. To compensate for the baby's nutritional deficiency, vitamin preparations are used. If fetal hypoxia is suspected, a woman is recommended oxygen cocktails.
If the cause of premature maturation of the “children’s place” is infectious diseases, in parallel with the standard regimen, the woman is prescribed appropriate treatment with antiviral or antibacterial drugs. For late toxicosis, diuretics are prescribed to reduce swelling, and drugs to lower blood pressure if the expectant mother has hypertension.

If systematic observations of the baby indicate the slightest negative changes in his condition, conservation therapy is canceled and emergency delivery is carried out. This is necessary in order to save the child's life.

You should give up smoking, alcohol, and uncontrolled use of medications in advance - antibiotics, anticonvulsants, hormonal drugs, including contraceptives, are especially dangerous.
If a woman is being treated with such drugs or is protected using oral hormonal contraceptives, before conceiving a baby, you should consult a doctor and take the necessary tests to avoid problems in the future.

From the first weeks of pregnancy, it is important to monitor your diet, avoid contact with toxic substances, radioactive radiation, and not work night shifts, since lack of sleep leads to hormonal imbalance. When bloody discharge at any stage, you need to consult a doctor to rule out placental abruption, and get the necessary treatment if it occurs.
A woman should breathe fresh air, walk if the weather permits, and sleep with the window open. The more oxygen she gets herself, the more she can give it to her baby through the placental bloodstream. You should also avoid viral infections by carrying out correct and timely prevention of influenza and ARVI, especially during periods of mass morbidity.
The placenta (baby place) is an embryonic organ responsible for supplying the fetus with oxygen, nutrients, as well as immune protection and excretion of waste products. This organ is formed at the 12th week of pregnancy from the lining of the uterus - the endometrium - and fibrin cells of the embryo. Many people confuse the placenta and the umbilical cord, but these are completely different organs.
The placenta looks like a flat vascular formation weighing 0.5-0.6 kg and up to 200 mm in size. The baby's place is usually attached to the upper or back wall of the uterus, connecting to the fetus through the umbilical cord. Maternal blood with oxygen and nutrients enters the placenta, and from it passes through the umbilical arteries and veins to the fetus.
What is placental aging?
The embryonic organ ages naturally, which is due to the physiological processes of gestation. But due to various unfavorable factors, this process begins prematurely, which in some cases negatively affects the child. Outwardly, early maturation does not manifest itself in any way, and aging can be diagnosed during an ultrasound.
What does “aging placenta” mean? The aging process of an embryonic organ is the depletion of a resource when changes occur in the density, structure, thickness and area of its tissues and vessels. Any deviation in morphology serves as the basis for a diagnosis of “premature aging”.
Stages of aging
In its natural state, the baby's place reaches maturity at 37 weeks, after which its blood supply function begins to decline.
Gynecologists diagnose four degrees of aging of the child's place:
- 0 – if the organ maintains normal structure and function until week 30;
- 1 – slight modification of the structure, detected from 27 to 34 weeks;
- 2 – resource exhaustion from 35 to 38 weeks;
- 3 – pronounced aging after 37 weeks.
The discrepancy between the structure and function of the child's place and the gestational age may vary. The more pronounced the changes in the structure in the early stages, the more dangerous this condition is for the child.
From 12 to 30 weeks, the baby's place develops along with the fetus, at this time an extensive network is formed blood vessels for sufficient supply developing child nutrients. Normally, it fully matures by 30-32 weeks, after which calcium deposits and other morphological signs of resource depletion appear on the walls of blood vessels. During childbirth, the so-called “death of the placenta” occurs: it is separated from the wall of the uterus and comes out after the expulsion of the fetus. Once released, the baby's place is called the placenta.
Helpful comments from the doctor in this video:
Why does the placenta age?
Accelerated maturation occurs as a result of various factors on the part of mother and child:
- multiple pregnancy - carrying twins or triplets;
- hormonal disorders - deficiency of chorionic hormone, deficiency of the progestin component;
- oligohydramnios or polyhydramnios – insufficient or excessive amount of amniotic fluid;
- damage to the walls of the uterus as a result of abortion, surgery, trauma or pathological childbirth in the anamnesis;
- late motherhood (after 35 years);
- complicated pregnancy (preeclampsia);
- Rhesus conflict - incompatibility of the blood groups of mother and child;
- chronic sexually transmitted infections in the mother (herpes, toxoplasmosis, chlamydia);
- reduced immunity, chronic respiratory infections in a pregnant woman;
- other chronic diseases in women (renal failure, diabetes, hypothyroidism).
Theoretically, any pathological processes in a pregnant woman’s body can lead to premature exhaustion of the embryonic organ’s resource. This occurs especially often due to pathology reproductive system. Previous sexually transmitted infections, surgical abortions, uterine curettage for medical reasons, trauma and surgery on the pelvic organs in a woman lead to scarring of the inner surface of the uterus. This disrupts the blood supply to the endometrium during placentation and limits the natural resource of the child's place.
The dangers of early maturation of the placenta
Premature maturation of a child's place does not always mean danger for the child. If the morphology of tissues and blood vessels corresponds to the duration of pregnancy, then doctors usually give a favorable prognosis. Resource depletion at 36-37 weeks, corresponding to 2-3 degrees of aging, is a normal physiological process.
If the expectant mother is healthy, then placental insufficiency is not diagnosed, because Compensatory mechanisms are activated in the woman’s body. If no abnormalities are observed during ultrasound intrauterine development fetus, then minor changes in the structure do not require correction.

What are the dangers of pathological placental insufficiency caused by premature maturation? At week 20, 2 or 3 degrees of maturity are already dangerous for the unborn baby. Pathology is understood as a clear discrepancy between the size and morphology of an organ and the gestational age. Since it is responsible for supplying the child with oxygen and nutrients, the degenerative process is potentially dangerous.
Ripening ahead of time leads to various consequences:
- chronic hypoxia (oxygen starvation) of the fetus;
- premature placental abruption;
- early discharge of amniotic fluid;
- developmental abnormalities in a newborn;
- premature birth.
At stages 0-1, aging can be corrected at 22-25 weeks. By detecting early maturation in time, the doctor can reduce the negative consequences for the child. At stages 2-3, as a result of early aging of the embryonic organ, the child experiences hypoxia, which is fraught with mental and/or mental disorders. physical development. In this case, induction of labor is indicated provided that the fetus is viable before the due date.
How to Diagnose the Problem
The problem with diagnosing premature ripening of the placenta is that it cannot be detected by any signs. It can be indirectly assumed by changes in the motor activity of the fetus. As a result of hypoxia, the child begins to move more actively or, conversely, practically freezes.
The diagnosis can be confirmed only on the basis of an ultrasound examination, which detects changes in thickness and area or in its structure. Doppler ultrasound, cardiotocography (examination of the child’s heartbeat), and biochemistry of blood taken from the umbilical cord are more informative. The doctor can determine the accelerated aging of the child’s place by the condition of the fetus. If there is chronic hypoxia and nutritional deficiency, then the fetus may have a smaller size that does not correspond to the gestational age.
Treatment methods
It is impossible to restore the structure of a child's place or prevent its further degeneration. Treatment of precocious ripening is aimed at compensating for the deficiency of oxygen and nutrients in the child.
What can be done to improve fetal nutrition and compensate for the lack of nutrients and oxygen? The expectant mother is prescribed medications that increase blood flow and improve oxygen supply. Vitamin and mineral complexes are also prescribed to improve the nutrition of the child’s body.
In parallel with vitamins and minerals, the factors that caused the pathology are corrected. For example, an expectant mother in a hospital is prescribed antiviral and antimicrobial drugs if a genital tract infection was detected during the examination.
Features of pregnancy and childbirth with this diagnosis
Rapid depletion of a resource does not always negatively affect gestation and delivery. Premature aging after 33-25 weeks practically does not determine the outcome of pregnancy and childbirth. Even stages 2 and 3 of maturation give almost the same prognosis as with healthy pregnancy.
In other cases, complications arise. If the embryonic organ begins to age before the 27th week, then an ultrasound may show fetal hydrops, underdevelopment of the limbs and internal organs resulting from nutritional deficiency. Severe abnormalities in intrauterine development are a provoking factor for miscarriage.
Sometimes premature maturation of the child's place indirectly affects the outcome of pregnancy and delivery. For example, as a result of hypoxia, the baby may move excessively in the womb, which leads to entanglement in the umbilical cord and complications during childbirth.
How to prevent premature aging of the placenta - prevention
It is possible to prevent early maturation of the child's place during planning of conception, as well as in its early stages. This condition is easier to prevent because There are no methods for “rejuvenating” the placenta. Knowing about the existing risk, the expectant mother, before conception, needs to be examined by a gynecologist for hidden sexually transmitted infections, because They are the ones that most often cause accelerated aging. Antiviral or antimicrobial therapy is acceptable in early pregnancy. Treatment medications must be prescribed by a doctor.

Six months before the expected conception, if there are chronic diseases, a woman should undergo a course of treatment. Particular attention should be paid to the condition of the kidneys, thyroid and pancreas, as well as the hypothalamic-pituitary complex, ovaries and adrenal glands. Women suffering arterial hypertension, are at risk of polyhydramnios, increased uterine tone, which leads to placental insufficiency. Therefore, it is advisable to start a course of antihypertensive therapy before conception in order to reduce the risk of gestosis in the middle of pregnancy.
Practice shows that regular intake of perinatal vitamin and mineral complexes reduces the likelihood of early depletion of resources.
Conclusion
Aging of the placenta is a natural process that begins after 30-32 weeks. The organ that supplies the baby with oxygen and nutrients exhausts its resources by the 39th week. This natural process ends with the “death” of the placenta, which is released as an afterbirth during childbirth.
In a healthy pregnancy, doctors do not classify early maturation of the embryonic organ as a pathological condition. But if the process begins before the 27th week, then with 2-3 degree aging, chronic fetal hypoxia occurs. It is fraught with the birth of a child with underweight, mental and physical developmental disabilities. In a pathological pregnancy, if the fetus is viable, labor is stimulated.
Premature aging of the placenta is a pathological condition that occurs during pregnancy. Briefly about what the placenta is. This is an organ that exists only in female body during pregnancy. The placenta provides the connection between mother and child.
Its history begins from the moment the fertilized egg attaches to the wall of the uterus (this occurs within 2 weeks after fertilization).
From this moment on, the child and mother have a joint circulatory system, through which the growing body receives all the necessary substances and removes its waste products.
This is how the fetus eats and breathes. In addition, the placenta performs a barrier and protective function - only substances and immune complexes from the mother’s blood that have passed the hematoplacental barrier reach the baby.
But you shouldn’t rely on this function of the placenta for everything: many toxic substances and pathogens easily pass the hematoplacental barrier.
The placenta goes through a number of stages in its development. From the beginning of its formation, it actively works, carrying out the above functions and producing hormones to maintain the hormonal status of pregnancy. Over time, “reverse development” begins in the placenta. Normally, the placenta grows until 35-37 weeks of pregnancy; after this period, the placenta may not change or become thinner.
Each period of pregnancy has its own ultrasound picture of the state of the placenta - the degree of maturity.
Premature aging of the placenta is a condition in which ultrasound examination reveals a degree of maturity of the placenta that does not correspond to the gestational age. The examination takes into account the thickness of the placenta, the state of blood circulation in it, and some other factors.
During a normal pregnancy, the maturation of the placenta proceeds as follows:
-1st degree – 27-34 weeks of pregnancy;
-2 degree – 32-39 weeks of pregnancy;
-3 degree – starting from the 36th week.
Thus, premature aging of the placenta is diagnosed in cases where the second degree of maturity appears at less than 32 weeks, and the third at less than 36 weeks.
This condition poses a certain threat to the course of pregnancy and the development of the child, but modern means of drug correction make it possible to avoid complications.
Premature aging of the placenta can develop under the influence of many factors: - history of abortion,
– diseases of the endocrine system,
– other chronic diseases of the mother,
-smoking,
-Rh-conflict,
– gestosis, etc.
If such a pathology is detected, you should not panic: about a third of pregnant women have the described condition and this does not prevent them from giving birth to a healthy baby normally. Listen to the recommendations of the gynecologist who is observing you and follow all instructions.
The placenta is a special organ that originates and grows in the uterine cavity during pregnancy, the main task of which is the correct connection of the blood supply systems of the fetus and matter. In the body of the placenta, biochemical processes take place that are responsible for the normal development of pregnancy, for the production of special hormones that provide the fetus with oxygen, and also protect it from the influence of harmful factors. After the birth of a child, the baby's place dies and separates 30 - 50 minutes after birth.
Degrees of placenta maturity at different stages of pregnancy
Like any organ, the placenta has its own “age,” that is, it is born, develops and matures, and then ages and dies after childbirth. This is a normal physiological process, however, early, premature maturation or aging of the placenta poses a threat to the health and life of the baby.
Currently, in obstetric and gynecological practice, four stages of placental maturation are differentiated, and each of them normally corresponds to a certain period of pregnancy.
However, there are so-called transitional stages when signs of adjacent degrees of maturity may appear, which is associated with different rates of development of the fetus and placenta, which occurs from its edges to the center.
- 0 – zero degree of maturity (according to the classification of Grannum P.A. 1979) can be diagnosed up to the 30th week;
- 0 – I degree (transitional period) is typical for weeks 29, 30;
- I – the first degree of maturity is observed at 30–32 weeks;
- I – II (transition period) is diagnosed at 32 – 34 weeks;
- II – the second degree of maturity corresponds to 34 – 40 weeks;
- II – III (transition period) can last from 35 to 40;
- III - third degree of maturity is diagnosed at 37 - 38 weeks to 40.
If pregnancy proceeds correctly, placental growth is completed by 36–37 weeks. After this, the thickness of the body of the child's seat decreases or does not change. Ultrasonic method examination (ultrasound) allows you to determine the thickness of the baby's place and the degree of its development, which is directly related to the state of the chorionic membrane (chorionic membrane surrounding the fetus and lining the fetal surface of the placenta), parenchyma (villous outer membrane of the embryo) and basal layer (connective tissue of the mucous membrane uterus).
Changes in the structure of the placenta at different stages of pregnancy
At 0 degree of development of the placenta, its structure is homogeneous. The chorionic membrane is flat and smooth, without undulations. The basal layer is not defined.
If the zero degree of maturity changes to degree I before reaching the 27th week, this indicates premature development of the placenta. As a rule, this condition occurs in the presence of negative factors: viral diseases such as rubella, chickenpox, suffered during pregnancy, smoking, drinking alcohol and drugs.
During the period of I degree At maturity, the growth of the placenta stops, and the body of the placental substance becomes thicker, and individual hyperechoic zones can be found in it, clearly visible during ultrasound examination; the chorionic plate becomes uneven. If at this time the doctor determines the II degree of maturity, this may be a sign of possible developmental disorders. In this case, it is necessary to take medications that activate blood flow in the vessels of the child's place.
At stage II of maturity (35–39 weeks), multiple echo-positive small inclusions are observed during ultrasound, the roughness of the chorionic plate increases, but its depressions do not reach the basal layer. In the basal layer itself there are small echogenic zones located linearly (the so-called basal “dotted line”). This stage of pregnancy is the most calm and stable. And even if in the middle of this period a pregnant woman is diagnosed with stage III maturity, this does not often become a cause for alarm.
Stage III is usually observed at 37–38 weeks, when the placenta reaches the final phase in its development and corresponds to the period of a normal full-term pregnancy. This period is characterized by the biological aging of the placenta, the structure of which becomes lobar, and the depressions of the chorionic membrane reach the basal layer. This stage requires a detailed analysis of any inconsistencies observed in the body of the placenta, since even minor deviations from normal development can be signs of threatening complications. If diagnosis at stage III of development indicates fetal hypoxia, then management of labor using surgical intervention (caesarean section) is often recommended.
Premature aging of the placenta
Premature aging of the placenta is noted in cases where stage II appears before 32 weeks, and stage III before 36 weeks. This is not yet evidence of pregnancy pathology, but requires mandatory monitoring of blood flow in the vessels of the uterus and baby’s place.
In the case of premature maturation of the child's place, a special protein is deposited on the villi, which is released from the blood circulating between them and prevents their participation in the metabolic processes of the uterine and placental blood flow. At this stage, by the end of 39–40 weeks, a decrease in the thickness of the placental membrane is recorded from 25 to 6 μm. Dystrophic changes are observed in the tissues of the placenta; lime salts settle in certain areas.
If the degree of maturation does not correspond to the duration of pregnancy, for example, when it should be I according to the weeks of pregnancy, but it is stated to be II, or at 33 weeks the III degree is detected, then a natural question arises: What is the danger?
The placenta, as one of the most important links in a single biological system that unites the fetus, the umbilical cord and the mother’s body, works on many life problems:
- Provides oxygen to fetal tissue cells and removes carbon dioxide from the blood;
- Delivers to cells nutrients and removes metabolic products;
- It is a barrier and filter that protect the embryo from the negative effects of harmful substances entering the mother’s body: drugs, toxins, bacteria;
- Produces hormones necessary for the proper development of pregnancy.
Therefore, premature aging or death of areas of the child's place negatively affects these functions. Deterioration of blood flow in the vessels of the uteroplacental system when the maturity of the placenta does not correspond to the established weeks of pregnancy is dangerous for the development of placental insufficiency, leading to hypoxia and malnutrition of the fetus, and in the worst case, intrauterine death.
Causes of premature aging of the placenta.
The most common reasons:
- Nicotine, alcohol and drugs that poison the cells of a child's place.
- Diabetes mellitus, thyroid disease.
- Hypertension in a pregnant woman.
- Late toxicosis (preeclampsia).
- Mother's blood is Rh negative.
- Previa and early placental abruption.
- Multiple births.
- Endocrine disorders.
- Multiple births.
- Intrauterine infections.
Late maturation of the placenta, causes and consequences
Such a diagnosis in the practice of pregnancy and childbirth is less common than the determination of premature maturation of the placenta. The main reasons for this status of a child's place are:
- primary and secondary diabetes mellitus in pregnant women;
- negative Rh factor leading to Rh conflict;
- chronic diseases of the expectant mother;
- smoking during pregnancy;
- alcohol consumption;
- fetal malformations.
If the development of the placenta is delayed and its maturation is late, we can say that it does not fulfill its mandatory functions - providing the baby with oxygen and the nutrients necessary for its proper development. In addition, carbon dioxide and metabolic products are retained in the fetal body, which contributes to its intoxication and leads to developmental delays.
The prognosis for a diagnosis of “late maturation of the placenta” is in most cases unfavorable without qualified medical treatment in a hospital setting. Otherwise, there is a high risk of stillbirth and mental retardation in the fetus.
Thus, the maturation of the placenta, its development, aging and death are natural processes, but the syndrome of premature aging and late maturing require special attention. Modern methods Studies of blood flow in the fetal-placental system have shown that an expanded analysis of its circulation allows the attending physician to make an accurate diagnosis.
And this makes it possible to prescribe the most effective treatment, choosing the optimal tactics for pregnancy management and obstetric care in order to achieve their favorable completion and the birth of a healthy child.
The placenta is called an embryonic organ, which is very important for the protection and development of the fetus. Its formation begins immediately after fertilization. The placenta ages naturally, reaching maturity by 37 weeks of gestation. In some cases, early aging of the placenta is observed; this condition is dangerous and requires treatment.
General characteristics of the phenomenon
The placenta begins to form approximately 12 days after conception, when the egg attaches to the wall of the uterus. During this period it is called chorion.
The formation of the placenta continues for the first 3 months, then it grows until the 8th month, after which the process of aging begins. This order is natural.
Aging of an organ means that its functional abilities decrease. This condition is dangerous, since the placenta is necessary to protect the fetus from infection, external damage, and ensure the supply of oxygen and nutrients.
It is fair to note that the ripening of the placenta ahead of schedule is quite rare. In some cases, such a diagnosis is made erroneously due to the incompetence of the doctor or incorrect interpretation of the examination results.
The maturation of the organ occurs in stages. Each stage has specific deadlines:
- 0 degree. The beginning of this stage is timed to coincide with the formation of the placenta, and it continues until 27-30 weeks.
- I degree. At this stage there is active growth of the placenta. It lasts approximately between 30-35 weeks.
- II degree. This period is considered the maturity of the placenta and lasts at 35-39 weeks.
- III degree begins after 39 weeks. The completion of this stage is childbirth.
Pathological aging of an organ is when stage II is diagnosed before 35 weeks or stage III before week 39.
Early maturation is also often observed, when the first degree of aging of the placenta began at 27-29 weeks. This phenomenon can be considered the norm, but the further process of maturation of the organ and the compliance of subsequent degrees of aging with the deadlines established for them should be monitored.
Week 21 is often called the equator. At this stage, the placenta should be well formed and strengthened. The thickness of its walls should be approximately 23 mm, but not more than 30 mm.
At week 22, the thickness of the placenta should increase to 24 mm. If it exceeds 30 mm, then there is a risk of premature aging.
Subsequently, the thickness of the placenta walls should increase by 1-1.5 mm per week, reaching 36.5 mm by week 36. The maximum permissible upper limit at this period is 46 mm. If the thickness of the placental walls increases more than normal, then there is a risk of premature aging of the organ.

Reasons
Organ aging earlier due date is a deviation from the norm. This condition can be caused by many factors:
- endocrine disorders;
- placenta previa, its partial detachment;
- low or polyhydramnios;
- infection;
- multiple pregnancy;
- exposure to toxic substances;
- gestosis (complication during pregnancy);
- impaired blood clotting;
- Rhesus conflict;
- chronic kidney disease, cardiovascular system;
- bad habits.
Premature aging of the placenta can be caused by either one of these factors or a combination of them. For proper treatment, it is important to identify the exact cause of the pathology.
It is almost impossible to independently determine the pathology. This condition is asymptomatic.
The main measure for identifying aging of the placenta that does not correspond to the prescribed period is ultrasound scanning. Such an examination is normally carried out three times during pregnancy, but if there are any violations, it is resorted to more often. Ultrasound scanning is safe, so there is no need to worry about the consequences of its frequent use.
The scan reveals thickening of the walls of the organ and the presence of calcifications in it. These deposits interfere with the full functioning of the organ.
Another important sign of pathology during ultrasound scanning is the condition of the fetus. The baby may be delayed in development, and his heart rate may deviate from the norm. Ultrasound examination allows you to assess the size of the fetus and its individual parts. This is important for assessing the degree of development and identifying its compliance with the norm or deviation from it.
To confirm the diagnosis, a blood test (general and coagulogram) is also performed. To identify disturbances in uteroplacental blood flow, Doppler ultrasound is performed.
Additionally, fetal cardiotocography is often prescribed. This measure is necessary to control the condition of the fetus. The study allows you to determine whether it has enough oxygen and nutrients.

What are the dangers of premature aging of the placenta?
Maturation of the placenta ahead of schedule can provoke the development of fetoplacental insufficiency. In this case, the risk of miscarriage increases tenfold, since essential functions placenta. This is especially true for the blood supply, if it is disrupted, oxygen and nutrients reach the fetus in insufficient quantities. This leads to a delay in his development.
Hypoxia of the fetus against the background of early aging of the placenta can cause fetal asphyxia. In this case, due to lack of oxygen, antenatal death occurs.
Abnormal aging of the placenta poses a risk premature birth, since the body receives certain signals. This is dangerous because the fetus is not yet able to function normally, so the chances of a favorable outcome are significantly reduced. But true premature aging of the placenta is extremely rare.
Premature aging of the placenta does not necessarily mean a threat to the fetus. If the violations are minor and do not have a negative effect on the fetus, then there is no need to worry. In this case, treatment may not be required; it is enough to monitor further aging of the placenta and the condition of the fetus.
Ultrasound specialist Susidko E.N. talks about the stages of placental maturation, the causes and degree of danger of the pathology:
Treatment methods
If the placenta ages earlier than expected, treatment is necessary. It is carried out in a hospital setting.
The goal of treatment in this case is to normalize blood flow and support the vital functions of the fetus. To achieve the required result, an integrated approach is required, including the use of the following means:
- Droppers to prevent oxygen starvation of the fetus. Usually they resort to Curantil or Actovegin. These drugs are important not only for the prevention of oxygen starvation, but also for normalizing umbilical cord blood flow.
- Eufillin. This drug is a vasodilator and helps normalize metabolism in the placenta and microcirculation.
- Aspirin. Necessary for thinning the blood and improving blood supply.
If premature aging of the placenta is caused by infection, then appropriate drug therapy is necessary. To prescribe it, the pathogen is first identified.
The list of necessary medications can only be determined by a specialist, based on the diagnostics performed and individual characteristics a woman’s body and her pregnancy.
Even drug therapy is not able to reverse the process. Treatment is necessary to slow down the aging of the placenta, maintain its necessary functions and maintain pregnancy until a safe date of delivery.
If a pathology is detected, a pregnant woman must give up bad habits if she has not done so before. It is also important to strictly monitor your diet and daily routine, and spend more time outdoors.
Proper nutrition means avoiding fried, salty and smoked foods. It is better to steam food. Flour products and sweets should be excluded.
Stabilization of the psycho-emotional background is necessary. Stress and emotional overload should be avoided. If necessary, you can take sedatives. It is better to choose herbal remedies such as Persen or motherwort tinctures. Taking any medications should be discussed with your doctor.

Forecast
With timely detection of pathology and proper treatment, the prognosis is favorable. An important condition for this is compliance with the regime, proper nutrition and all doctor’s instructions. If these rules are followed, the birth will take place on time, and the baby will be full-term and healthy.
In most cases, with diagnosed pathology, drug therapy is sufficient. Severe complications may require premature delivery. This option is appropriate only in critical situations when the risk negative consequences is high, so there will be more benefit from the development of the fetus outside the womb.
Premature delivery is usually resorted to when the third degree of aging of the organ has occurred ahead of schedule. Childbirth is carried out by caesarean section.
Aging of the placenta is an inevitable and natural process, but it must occur in accordance with certain deadlines. Premature aging of the placenta can pose a threat to the health of the fetus, its normal development and even life. It is important to start treatment in a timely manner to maintain pregnancy and avoid possible complications.