Because the knee is such a complex joint, it is important that an athlete who has injured a knee takes a comprehensive approach to knee recovery. It is especially necessary to fully restore the powerful muscles around the joint before returning to sports activities that put a lot of stress on the knee. Without this supporting muscle system, the likelihood of re-injury is high /4/. Recovery must begin as early as possible to prevent loss of mobility and strength. Prolonged inactivity after an injury causes a lack of strength and mobility, which need to be restored before returning to sports activities. Delays in rehabilitation entail delays in returning to sports. After an injury that does not require surgery or prolonged immobilization, range of motion training can begin as soon as pain and swelling subsides—usually no later than forty-eight hours after the onset of symptoms of the injury, and often as early as twenty-four hours. Even after some surgeries - for example, after surgery for a torn meniscus - range of motion training in the knee should begin after twenty-four hours. For other surgeries, such as cruciate ligament repair, range of motion training can begin as early as five days after surgery, and no later than two to three weeks. The patient should be given a removable splint so that it can be removed during physical therapy, or an orthopedic fixation device that allows some movement. Exercise is the most successful way to restore an athlete to a state of readiness. A physical therapist may also use ice, surface warming, deep warming, massage, electrical stimulation, and physical manipulation of the knee to promote healing and make exercise more comfortable. The initial level of exercise intensity depends on the severity of the injury. Postoperative range of motion training usually starts at level one. At this stage, movement exercises are active, assisted - the physiotherapist helps the patient to use his own leg strength to move within acceptable limits. If the injury is too severe for this type of exercise, the patient can rely on passive exercises - the physiotherapist himself makes movements in the injured knee within an acceptable range. Exercise equipment providing continuous passive motion can be taken home by the patient so that he or she can do this type of range of motion training at home /10/. After the operation, the development of muscle atrophy is prevented by isometric exercises. Under the guidance of a physical therapist, these workouts can usually be started immediately after surgery.
Isometric exercises help maintain strength in the important muscles surrounding the knee without compromising healing processes because the length of the muscles remains the same. Athletes suffering from minor or moderate knee injuries may start with Level 2 exercises. On the initial stages rehabilitation program the main goal is to restore the range of motion in the joint; an additional goal is to prevent atrophy in the surrounding muscles. As the rehabilitation program develops, more and more strength exercises are included in it. Range of motion training should always be performed below the pain threshold. Any exercise that causes pain should be stopped /11/. Using the example of recovery after meniscus injury surgery, physical rehabilitation for injuries can be considered. knee joint in general, because general principles restores are saved. The urgency of the problem is confirmed by the high frequency of damage to the meniscus of the knee joint in athletes specializing in freestyle wrestling during the heyday of their sports activities. Damage to the meniscus of the knee joint is one of the most common types of pathology of the musculoskeletal system of athletes. Thus, according to studies, meniscal injuries account for 21.4% of the entire pathology of the musculoskeletal system. Most often, this type of damage occurs in athletes involved in martial arts (from 20.1 to 55.6%), playing (33.11%) and complex coordination sports (18.36%). The rehabilitation process after meniscectomy can be divided into three stages /12/:
I (sparing) stage of physical rehabilitation refers to the early postoperative period (2-3 days after surgery):
1) normalization of the trophism of the operated joint and relief of postoperative inflammation;
2) stimulation of the contractility of the muscles of the operated limb, primarily the thigh muscles;
3) counteracting physical inactivity, maintaining the overall performance of the athlete;
4) prevention of contracture of the operated joint.
The following tools are used to solve the tasks:
Treatment by position (the operated limb is placed in the average physiological position at a flexion angle of 135° on the Beler splint to create rest and reduce the tension of the joint capsule when inflammatory fluid accumulates in it);
The main form of physical rehabilitation is therapeutic gymnastics, which is carried out in the initial positions lying on the back, on the stomach, sitting, standing on a healthy leg;
From the 2-3rd day after the operation, in the absence of hemoarthrosis (synovitis), isometric tensions of the quadriceps femoris muscle are applied in the form of special exercises. The dosage of isometric tension of the thigh muscles at the beginning, after the operation is 1-2 seconds, and then 10-20 seconds. and 1-2 min. To prevent flexion contracture of the knee joint, in the absence of effusion in the joint, on the 6-7th day after the operation, the foot end of the bed is lowered;
Laying for extension of the operated joint is performed. To do this, a roller with a diameter of 5-10 cm is placed under the heel, so that the operated joint sags slightly. In this position, the athlete is 5-7 minutes, and then the duration of styling increases to 7-10 minutes. Laying is repeated 2-3 times. By the 10th day, it is possible to completely eliminate the flexion contracture. Remedial gymnastics includes general developmental exercises for all muscle groups. The duration of therapeutic exercises at the beginning is 15-20 minutes, and by the end of the recovery stage it reaches 30-40 minutes.
Therapeutic massage and other physiotherapeutic procedures should not be carried out, as they support the phenomena of synovitis.
II (functional) stage of physical rehabilitation (10-12 days after surgery):
1) elimination of contracture of the knee joint;
2) restoration of normal gait;
3) adaptation to long walking and household loads;
4) strengthening the muscles of the operated limb.
The following forms of physical rehabilitation are applied:
Therapeutic gymnastics in gym;
Physical exercise in the pool;
Walking training;
Self-study of athletes in the chamber for the implementation of motor tasks;
Exercises on a bicycle ergometer are also used for all muscle groups;
A special exercise is the semi-squat, which is performed in front of a mirror in order to control the even pressure of the load on both legs.
Duration of classes - 60 min. Classes are held 2 times a day /10/. Physical exercises in the pool are carried out at a temperature of +30°, +32°. The following exercises are performed in the water: walking, light exercises for the operated joint in order to eliminate the residual effects of contracture and strengthen the muscles of the thigh, gluteal region and lower leg, crawl swimming on the chest and back. Class time - 20-40 minutes.
Walking training is carried out: on the first day, at a pace of 80 steps / min, athletes walk 1 km in 10 minutes. Subsequently, the distance and walking time increase (up to 30-45 minutes).
III (training) stage of physical rehabilitation (16-18 days after surgery):
1) complete restoration of the function of the operated joint;
2) restoration of strength endurance and speed-strength qualities associated with the specifics of the sport.
The main means of rehabilitation are physical exercises, which in terms of volume, specificity and intensity are close to the initial stage of sports training. Physical exercises lasting up to 1.5-2 hours are held in the gym and in the pool. The classes include slow running at first on the treadmill, and after two or three workouts - slow running in natural conditions.
Athletes of the martial arts group perform simulation exercises taking into account the specifics of their sport /12/.
Studying the statistics of injuries of the musculoskeletal system, it turned out that injuries of the knee joint are the most common (about 50% of the entire pathology of the musculoskeletal system). Although the knee joint is quite large and relatively well protected, it remains very vulnerable to traumatic factors.
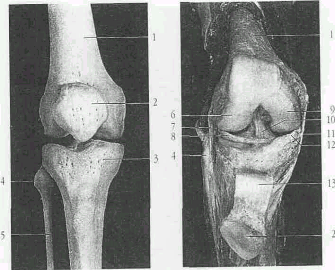
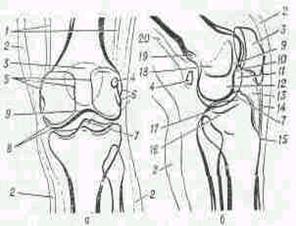
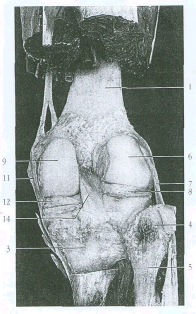
Anatomy of the knee joint
To understand the features of injuries and recovery after them, it is first necessary to have an understanding of the structure of the knee joint. The knee joint is the junction of the femur and tibia. In front of the joint is the patella, which is held by the patella ligament. The ligamentous apparatus of the knee joint is represented by the patellar ligament, lateral and medial ligaments, which strengthen the joint from the sides. The cruciate ligaments are inside the joint and prevent the tibia from moving. The surfaces of the joints are covered with articular cartilage, in the joint cavity there is a small amount of synovial fluid, which softens the friction of both surfaces of the joint. Between the articulation of the femur and tibia are the lateral and medial menisci, represented by falciform cartilages. The knee joint is surrounded by an articular bag.
Movements in the joint are represented by flexion, extension, and in a bent state - rotations around its axis.
Types of knee injuries
Athletes (football players, track and field athletes, hockey players, basketball players) often get knee joint injuries. The most common knee injury is meniscal injury. Damage to the meniscus takes about 21.42% of the total structure of injuries of the musculoskeletal system. The second place is occupied by damage to the bag-ligamentous apparatus, the internal lateral ligament is more often injured, less often the external one. In third place is damage. articular cartilage, it is often noted in athletes who perform jumping exercises (jumpers, dancers, figure skaters). Relatively rarely, a fracture of the patella with damage to its ligament is observed.
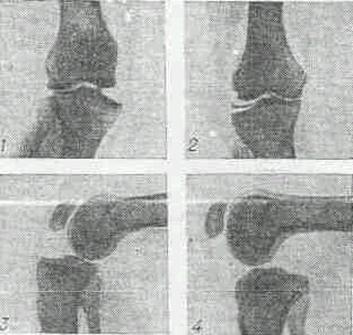
Diagnosis of knee injuries
The first diagnostic method is a clinical examination: collection of complaints, examination, palpation. Of the instrumental methods of examination, radiography of the knee joint is in the first place, it can be used to see a fracture of the patella and suspect a meniscus injury. Ultrasound examination of the knee joint allows you to verify the damage to the menisci. In controversial cases, the patient is offered to do computed tomography and nuclear magnetic tomography of the knee joints.
Phasesknee joint healing after injury
Consider the features of the restoration of the function of the knee joint after surgical interventions on it. Postoperative medical rehabilitation of the knee joint is divided into 4 phases:
The immediate postoperative phase (phase I). It is characterized by the presence of fresh postoperative wound, severe pain, atony of the quadriceps femoris muscle;
Early healing phase (phase II). This phase is characterized by a less pronounced sensation of pain, atony of the quadriceps femoris muscle at 90° flexion, and the presence of a reactive effusion;
Late healing phase (phase III). In this phase, there is no pain, there is no pronounced muscle atony, flexion is from 0 to 120°, moderate effusion is possible;
Phase of rehabilitation and recovery (phase IV). In this phase, there is full range of motion, partial muscle recovery, limitation of sports activity, and no effusion.
Periods of postoperative recovery of the knee joint
The early postoperative period lasts 2-3 weeks. In this period, the main goals are: to stop postoperative inflammation, normalize joint trophism, combat contractures of the knee joint, stimulate muscle contractility and maintain overall performance. The first place in the surgical hospital is occupied by drug therapy. Painkillers, antibacterial, decongestant and drugs that enhance regeneration processes are prescribed.
An important place, even in the first weeks after the operation, is occupied by physical rehabilitation. The primary means of physical rehabilitation in patients with injuries of the knee joint is therapeutic Physical Culture. Physical exercise in the affected limb stimulate blood flow, which in turn enhances regeneration processes and stimulates local immunity. Physical exercises in such patients are used in the form of:
Isometric tension of the femoral muscles of the operated leg;
Dynamic exercises of the operated leg in a gentle mode;
Therapeutic walking on a flat surface;
In order to maintain overall performance, it is recommended to perform general developmental exercises for the non-operated leg, arms and body;
Mechanotherapy (exercises on simulators) both for the operated limb and for undamaged parts of the body.
In the first days, classes in therapeutic physical culture are carried out for 20-30 minutes with a minimum load on the operated limb. In the early postoperative period, it is also advisable to use massage (manual massage, hydromassage, pneumomassage), physiotherapy (UHF therapy, electrical stimulation of the quadriceps femoris muscle). The effectiveness of such methods of physiotherapy as magnetic therapy and ultrasound, which increase microcirculation in the operated joint, reduce swelling and relieve pain, has been proven.
The recovery period lasts 6-8 weeks and solves the following tasks:
Restoring the optimal motor stereotype and increasing tolerance to physical activity;
Training of strength endurance of the muscles of the thigh, buttocks and lower leg;
Restoration of general working capacity;
Restoring the flexibility of the knee joint;
Psychological therapy.
Therapeutic physical culture is used in the following forms:
Mechanotherapy in the gym lasting 1 - 1.5 hours;
Dosed therapeutic walking and running.
The recovery and training period sets itself the following tasks:
Restoration of general and special fitness;
Adaptation to simple training loads;
Endurance training.
Of the methods of physical rehabilitation at this stage, they are used in the form of therapeutic physical culture, massage and physiotherapy. The motor regime at this stage is significantly expanded, mechanotherapy in the gym is carried out up to 5 times a week with the expansion of loads on the operated limb. In the recovery and training period, massage and manual therapy are successfully used, which help to increase the motor volume in the joints, strengthen muscles and eliminate muscle imbalance that occurs after a long forced position of the limbs and spine. During this period of recovery of the affected limb, from the methods of physiotherapy, electrophoresis, phonophoresis with various medicines, laser therapy and electrical muscle stimulation.
Criteria for assessing the restoration of knee joint function
The signs of restoration of the functional usefulness of the operated knee joint are the following tests:
Full range squat;
Walking in a full crouch ("goose walking");
Squatting in the operated leg (75% of the number of squats on a healthy leg is considered a good result);
Running for 30 minutes;
Ability to perform imitative and special preparatory exercises.
Consider the criteria for evaluating long-term results after knee surgery:
The result is considered excellent if the joint is stable, the range of motion is complete, the patient can perform any work.
Good results have the following characteristics: the joint is stable, the range of motion is complete, periodic pain, the patient can return to his work, the patient can go in for sports with some restrictions.
With a satisfactory result: the joint is stable, the range of motion is reduced by 15 - 20 °, frequent pain, the patient cannot engage in physical labor.
With an unsatisfactory result, the joint is unstable, pain is constant, swelling of the joint, limitation of the range of motion in the joint.
Having considered the features of recovery after knee injuries, I would like to say that the use of physical rehabilitation methods is no less important than the use of medications. And the active desire and participation of the patient himself in the recovery process is 50% of the success of the treatment.
2. Rehabilitation for knee injuries
An important role in the prevention and elimination of post-traumatic changes is played by physical exercises - specially organized for a specific purpose and strictly dosed movements. They are one of the important factors that support the vital activity of a healthy person and stimulate regenerative and compensatory mechanisms in the body of a sick person, since through the system of central regulations all adaptive processes are involved to ensure homeostasis.
I. P. Pavlov noted that movement is a natural function necessary for the existence of a person, affecting the entire body and relating to "the main reactive activity of the body." Regular exercise creates dominant foci of excitation in the cerebral cortex, which, by the mechanism of negative induction, leads to the suppression of foci of congestive excitation, i.e. eliminates "pain points".
The systematic use of physical exercises in the complex treatment of a patient eliminates the negative effect of hypodynamia on the body, and has a versatile beneficial effect. Rhythmic contraction and relaxation of skeletal muscles, tension and relaxation of tendons contribute to the improvement of venous outflow, the prevention of venous stasis, and the normalization of microcirculation in tissues. Physical exercise prevents the development of atrophy and degenerative changes in tissues and organs.
There are a number of factors that need to be taken into account when choosing an exercise therapy technique. The nature and severity of the injury, the stage of the pathological process, the physical and mental state of the patient, his physical fitness. A set of exercises should be compiled strictly individually, taking into account the phase of the process.
In the treatment of injuries of the musculoskeletal system, physiotherapy methods are widely used. IN early dates after injuries, UHF, ultrasound, magnetotherapy are used. This allows you to reduce swelling, improve microcirculation in the injured limb, and reduce pain. After the termination of immobilization, electrophoresis, phonophoresis with various drugs, laser therapy, electrical muscle stimulation are prescribed.
Massage and manual therapy allow you to strengthen the muscles, make them more elastic, restore or increase the range of motion in the joints, correct muscle imbalance that occurs after a long forced position of the spine and limbs.
Restorative treatment should begin as early as possible without waiting for fracture consolidation, immobilization or removal of sutures. Ideally, on the second or third day after injury or surgery. The earlier rehabilitation measures are started, the better the result.
Rehabilitation after dislocations and muscle tears of the knee is carried out approximately according to the same scheme as rehabilitation after fractures: it includes a course of physiotherapy, physiotherapy exercises, massages and the use of local ointments. When the cruciate ligament is ruptured, as a rule, it is not possible to do without surgical intervention.
Injuries to the meniscus of the knee joint and Koenig's disease are also treated in the majority by surgery. If the meniscus is damaged, the patient is prescribed arthroscopy - an operation that allows intra-articular surgical interventions to be performed without opening the joint cavity. Koenig's disease is usually treated by removing the affected area of the bone. In children and adolescents, a positive effect can also be achieved with conservative treatment, including the appointment of vascular drugs and drugs that improve nutrition and restoration of articular cartilage, as well as physiotherapy and exclusion. physical activity on the joint.
Deforming arthrosis of the knee joint is not amenable to conservative treatment. This disease has a chronic course, and the patient can be completely relieved of pain only with the help of arthroplasty - an operation in which the joint is replaced with a metal structure. In this case, rehabilitation will be the same as after a fracture.
Often, traditional methods of rehabilitation after injuries and fractures of the knee pull a person out of his usual way of life for a long time: he cannot move independently and is forced to forget about work for a long time and, possibly, even lose it. At the same time, he needs money not only no less, but much more than a healthy person, because serious and long-term treatment after fractures often requires large financial costs.
In addition, it is almost impossible for a person with a serious fracture to visit the clinic every day, so most patients have to hire private masseurs and exercise therapy instructors. Physiotherapy at home, as a rule, is not carried out.
Exercise therapy is complicated by the fact that
Rehabilitation after surgery on the joints can be divided into 2 main stages. An example is rehabilitation after surgical reconstruction of the anterior cruciate ligament.
When restoring the anterior cruciate ligament of the knee joint, it must be remembered that the ligament provides not only mechanical protection against instability of the knee joint (the feeling of “out” of the joint), but is also the most important receptor organ that informs the body about changes in the position of the joint in space, the speed of movement. Very often, with a partial rupture of the ligament and an improvement in the condition of the knee, the athlete begins training in full. However, the receptor function is not fully restored, the knee feels inadequate, which can lead to a complete rupture with a “normal” load. Therefore, exercises after surgery should include special techniques aimed at restoring this receptor function of the ligament. Muscle function must also be taken into account. So the inner wide part of the quadriceps femoris muscle, to the greatest extent, after any, even a minor injury or operation, is subject to rapid dysfunction and weight loss. Its functions are very important, as it is the only muscle that ensures the correct position of the patella (patella) when bending the knee. Even with a minor injury or diagnostic arthroscopy, incomplete recovery of this muscle can lead to severe dysfunction of the knee joint.
The rehabilitation program is compiled using a minimum and sufficient set of portable physiotherapy devices (for myostimulation, magnetotherapy) and special exercises.
Stage I - medical rehabilitation. Duration up to 4-6 weeks after surgery. Frequency of visits to the doctor 1 time in 1-2 weeks.
Main tasks:
1. Remove inflammation and swelling
2. Restore the range of motion in the joint.
3. Prevent violation of the biomechanics of the joint.
4. Protect the ligament graft and other structures of the knee joint.
5. Maintain muscle activity, strength and volume.
6. Prevent loss of coordination.
7. Optimize motor skill (walking training, basic functional movements).
Main tasks:
1. Increase speed-strength characteristics and muscle volume.
2. Improve coordination, balance.
3. Maintain the flexibility of joints, ligaments and muscles.
4. Correct motor stereotype.
5. Prepare for plyometric activity (jumps).
6. Start cyclic highly coordinated activity (running).
7. Train special motor skills (sports activity).
8. Objectify the result of the restoration (clinical tests, ligament stability, functional tests, biomechanical testing, magnetic resonance imaging).
The means that are used at the stages of rehabilitation mutually complement and enhance the positive effects of their use. The rehabilitation program allows you to maximize the quality of life in an optimal way. short time.
Literature
1. Dubrovsky V.I. Sports medicine: A textbook for university students. - M.: Humanitarian publishing center "VLADOS", 1998. - 480 p.
3. Sports medicine and therapeutic physical culture.: Textbook. for tech. physical culture./ Ed. A. G. Dembo. – Ed. 2nd, add. and reworked. - M.: Physical culture and sport, 1979. - 352 p.
4. A. A. Korzh, E. P. Mezhenina, A. G. Pechersky, and V. G. Ryndenko. Handbook of traumatology and orthopedics / Ed. A.A. Korzh and E. P. Mezhenina. - Kyiv: Healthy "I, 1980. - p. 216.
5. Physical rehabilitation. Textbook for students of higher educational institutions.: Ed. prof. S. N. Popova. Ed. Third revised and additional: Rostov-on-Don "Phoenix" .: 2005.
2 months Subsequently, if the failure of the ligamentous apparatus of the knee joint is revealed, it is plastically restored. Section 2. Physical rehabilitation for injuries of the knee joint 2.1. Fracture of the patella 2.1.1. Exercise therapy Classes in therapeutic exercises are carried out 2-3 times a day. The duration of classes in the first 2-3 days is 10-15, in the future - 20-30 minutes ...
The groups increased the pace of steps and estimated walking speed more significantly. All this indicates that the level of physical fitness achieved as a result of physical rehabilitation of patients after the treatment of ankle joint injuries contributed to the acquisition of more stable walking skills. In general, at the end of the pedagogical experiment, 7 patients of the control group walked ...
The joint is prescribed a course of mechanotherapy, the procedures of which are advisable to be carried out after paraffin, ozocerite or mud applications, as well as after therapeutic exercises or classes in the pool. 2. Physical rehabilitation for injuries of the ligaments of the knee joint Injuries of the knee joint are very diverse: from damage to the ligament-tendon apparatus and joint capsule, patella, to ...
5-20 minutes daily or every other day. For burns, an underwater shower-massage is effective. Section 4 Practical work Treatment of patients with burns using conservative methods of rehabilitation 4.1 Relevance of the topic The problem of rehabilitation of victims of burns deserves close attention. Wide circle doctors are little familiar with the organization of care for burn convalescents, with the possibilities ...





