As an X-ray surgeon, I would like to dwell on the technique of percutaneous transhepatic decompression. bile ducts with a malignant nature obstructive jaundice.
Percutaneous transhepatic cholangiography - conditions for performing, advantages and disadvantages of the method.
A prerequisite for performing percutaneous puncture is the expansion of the intrahepatic bile ducts up to 3-5 mm. With obstructive jaundice of any etiology, this phenomenon is quite common, in case of violation of the outflow of bile, it begins to accumulate primarily in the ducts, gradually expanding them. If the obstacle (stone or tumor) does not completely compress the choledochus, i.e. part of the bile still flows into the intestine, this process may take some time.
The data for cholangiocarcinoma are hardly more favorable. Therefore, there is an important palliative approach to these cancers, which concerns the vast majority of patients. The initial evaluation of these tumors is important as it should establish the resectivity of the tumor, which consists of clinical examination and imaging. Surgical bypass and endoscopic or transepatic biliary replacement usually allow regression or resolution of jaundice. If these methods do not improve survival, the quality of life of patients improves.
Advantages of the method:
- Performed under local anesthesia (i.e. does not require general anesthesia)
- In experienced hands, the success rate of drainage is 98-100% (which exceeds the technical success of endoscopic methods).
- Fewer complications (with the necessary equipment and experienced professionals).
Disadvantages of the method:
Endoscopic derivation is generally preferred over other methods due to lower morbidity and early mortality, even if surgical output is less. However, recent advances in endoscopic techniques, in particular the use of biliary and digestive metal prostheses, should further improve outcomes and should this statement is in perspective. Finally, the only sure sign of surgical derivation is in patients with a tumor that is determined to be resected, and in whom intraoperative results lead to the rejection of curative surgery.
- Performed under fluoroscopic guidance (although modern equipment allows you to reduce the radiation dose to the minimum figures - less than when performing computed tomography).
- When installing external or external-internal cholangiodrainage, part of the bile flows into a special Plastic container, which must be carried with you from 3 to 14 days, which worsens the patient's quality of life.
In the hospital, patients with obstructive jaundice are admitted to the departments of surgery/oncology. As a rule, operations aimed at decompression of the bile ducts are urgent - i.e. urgent enough to avoid complications associated with bilirubin intoxication, but also not performed immediately upon admission of the patient. Usually, doctors have 1-3 days for additional examination of the patient - establishing the cause of jaundice (stone, tumor, stricture), determining the level of bilirubin in the blood, and other tests that must be taken into account when preparing for surgery.
The incidence of symptomatic obstruction of the second duodenum requiring bypass is between 5% and 20% depending on the series, so it is doubtful to systematically suggest a double conclusion at the time of diagnosis, but it is certainly indicated in the 10% of so-called able-bodied patients who have tumor inoperable at laparotomy. The morbidity and mortality of the surgical procedure performed later in evolution are high, now in the case of late duodenal obstruction, endoscopic or radiologically large metal metal prostheses can be used.
The patient is explained the purpose of the operation, its risks and possible complications signed voluntary informed consent for the procedure. On the eve, a light dinner is allowed, on the day of the intervention - hunger.
Percutaneous transhepatic drainage in cancer of the pancreas and bile ducts.
 Operations of percutaneous transhepatic cholangiodrainage (PCCD) and stenting are performed in a specially equipped X-ray operating room.
Operations of percutaneous transhepatic cholangiodrainage (PCCD) and stenting are performed in a specially equipped X-ray operating room.
These duodenal metal prostheses are being evaluated, but early results seem encouraging in the short term. Extrahepatic cholangiocarcinomas, i.e. all malignant tumors that have developed from the bile ducts from the liver sleeve to their place in the duodenum account for about 5% of all cancers digestive system. "in-hospital obstruction is most often metastasis of another cancer, extension of hepatocellular carcinoma, or cancer of the vesicle." Often the diagnosis is late, now they benefit in terms of evaluating the expansion, progress carried out in the radiological examination of the bile ducts.
The intervention is performed under local anesthesia, usually 20-30 ml of 1% lidocaine solution. In the conditions of our hospital, an anesthesiologist-resuscitator is always in the operating room, who, if necessary, provides intravenous anesthesia.
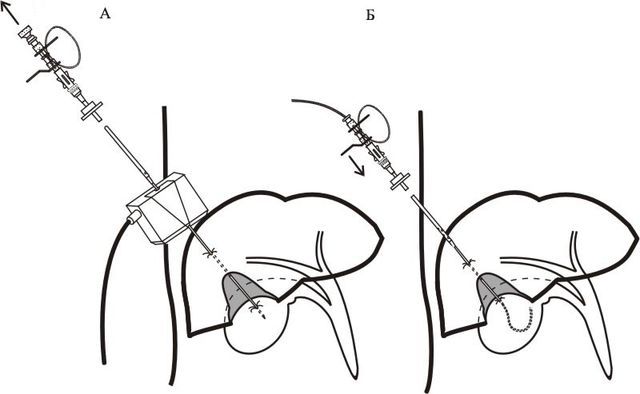
The puncture site is selected individually, depending on the anatomical structure and localization of the obstacle. As a rule, access to the ducts of the right lobe of the liver is carried out from the 7th-8th intercostal space along a line drawn perpendicularly from the anterior angle of the armpit. Access to the ducts of the left lobe - from under the xiphoid process.
Curative resection is the only therapeutic option that provides a significant improvement in survival, with a median survival of 3 years if the removal was completed. resectability of the tumor, most authors invite the practice of careful selection for various indications.
Without any treatment, most patients with malignant bile duct obstruction die within 3 months of the onset of jaundice. Although only surgical treatment remains curative, for cholargiocarcinoma, most patients do not work at the initial presentation of their disease. In a series of 552 extrahepatic bile duct cholangiocarcinomas in 307 patients with intrauterine activity, therapeutic resection was performed in only 32% of cases.
The correct choice of access to the greatest extent affects the safety of the technique.
How is the operation of drainage of the bile ducts?
After treating the skin with an antiseptic solution and anesthesia, the skin at the puncture site is incised with a scalpel to facilitate insertion of the puncture needle. The needle itself has a diameter of less than 1 mm. Under the control of ultrasound or fluoroscopy, it is carried out to a depth of 5-10 cm until it enters the dilated bile duct.
For the palliative treatment of cancerous tumors in chest there are no data from the literature that compare prospectively different endoscopic, radiological and surgical methods. Methods of non-surgical drainage are based mainly on long-term percutaneous drainage and placement of endoprostheses radiologically or endoscopically. Long-term percutaneous drainage, in addition to the preoperative interest discussed above, may be a treatment for cholestasis, but it is subject to mechanical complications such as drain removal.
It also imposes restrictive care maneuvers and is responsible for significant patient discomfort, contrary to the goals of palliative care. Comparison of two large groups of patients treated non-surgically for malignant crunch obstruction, one endoscopic and the other percutaneously, illustrates the previous finding. In contrast, percutaneous drainage appears to be more effective in reducing jaundice with fewer infectious complications, while mortality was lower by one month in the radiological series, which can probably be explained by drainage. initial more complete.
A few milliliters of a non-ionic iodine-containing contrast agent (omnipak, optirey) is injected through the needle. This is done in order to make sure that it enters the bile duct, and not the vessels of the liver. A thin soft conductor with a diameter of up to 0.3 mm is inserted through the lumen of the needle, the needle is removed, and a thin plastic catheter (less than 2 mm in diameter) is inserted through the installed conductor. Through it, 20-30 ml of a contrast agent is injected - the so-called. cholangiography.
In addition to the fact that these series are not strictly comparable, these data from the literature are relatively old and endoscopic drainage techniques have improved especially now, especially in control centers. if the study is currently being carried out in best conditions, in most cases it is possible to insert two wires, stretch the stenoses, then place the two prostheses in parallel, merging the right liver and left liver. It is well known that the more complete the drainage, the better the short and long term results.
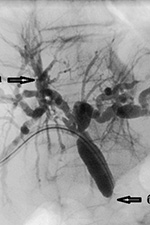 |
Rice. 3. Percutaneous transhepatic cholangiography. Defined: With regard to the choice of type of prosthesis, the problem of biliary malignant stenosis is different from the problem of submandibular stenosis. Plastic prostheses may be preferred when it comes to patients with life expectancy, in which multiple parallel prostheses sometimes occur. In addition, in the case of subsequent expansion of the tumor, requiring additional drainage, its metal prostheses may be difficult. The first point is to make sure that the patient is not lucky, that he can benefit from the treatment surgical treatment. Where there are extensive lesions, metastases, or poor prognostic factors, only palliative management may be considered, non-surgical management of jaundice and pruritus. The most reasonable palliative attitude is the placement of an endoscopic prosthesis. |
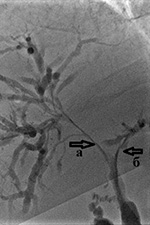 |
Rice. 4. Cholangiography for obstructive jaundice caused by Klatskin's tumor. A pronounced narrowing of the right (a) and left (b) lobar bile ducts is determined due to the germination of cholangiocarcinoma |
Tight filling of the bile ducts allows you to accurately determine the level and degree of blocking of the bile ducts, the degree of their expansion, defects in their filling (large calculi and intraluminal tumors are visible), as well as determine the tactics and method of further treatment - decompression of the bile ducts.
The liver performs several functions, including the production and storage of substances needed to sustain life. It deals with toxic substances and plays a role in the elimination of these processed toxins. It produces bile, which contains the substances necessary for the digestion of food. Bile is temporarily stored in the gallbladder and reached the small intestine via the main bile duct, usually in response to a stimulus such as eating a fatty meal. Processed toxic substances are transported into the bile.
These processed toxic substances are removed when a person empties their intestines. When "bile is obstructed, red blood cells can s" accumulate and cause a yellowish discoloration of the skin and "other mucous membranes of the body as white off" the eyes and the underside of the tongue. Obstruction to the flow of bile is usually caused by stones in the bile duct. The origin of these stones may be in the gallbladder or in the bile ducts. Most of these stones can be treated endoscopically. A small proportion of the stones, however, must be removed surgically.
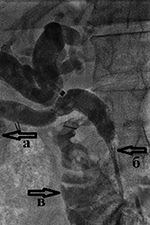 |
Rice. 5. Cholangiography for intrahepatic cholangiolithiasis: A) multiple small stones (stones) up to 2-3 mm in size inside the dilated bile ducts of the right lobe of the liver; Other main causes of biliary obstruction are in particular the narrowing of the bile ducts as a result of "inflammation caused by calculations, lesions of the bile ducts caused during surgery" gallbladder ablation and cancer of the bile duct, pancreas or upper small intestine, called the duodenum Surgical ablation, in is currently the only remedy available for these cancers. These operations are usually large operations. Some surgeons perform temporary bile drainage procedures before performing a major procedure to relieve a bile duct obstruction caused by stones, inflammation, or cancer. |
Bile obtained from primary bile duct puncture is often taken for culture and antibiotic susceptibility testing. This greatly contributes to the fight against such a frequent complication of obstructive jaundice as cholangitis - i.e. inflammation of the wall of the bile duct.
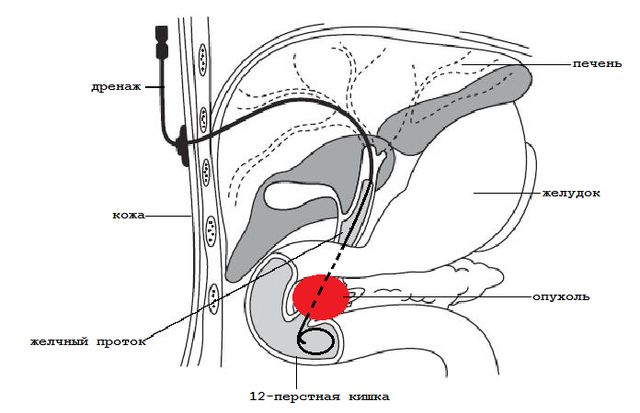
 After determining the level of the block, the doctor, using catheters of various shapes and conductors of different stiffness, performs recanalization of the obstacle (the conductor through the stricture or the choledochus squeezed from the outside is passed into the small intestine). A plastic tube with a diameter of about 3 mm is inserted through the conductor into the intestine to restore the outflow of bile. big amount holes - drainage.
After determining the level of the block, the doctor, using catheters of various shapes and conductors of different stiffness, performs recanalization of the obstacle (the conductor through the stricture or the choledochus squeezed from the outside is passed into the small intestine). A plastic tube with a diameter of about 3 mm is inserted through the conductor into the intestine to restore the outflow of bile. big amount holes - drainage.
These preoperative procedures may be performed endoscopically or under x-rays or other forms of imaging guidance through the liver. Other surgeons, however, believe that temporary bile drainage procedures are not needed and that the procedure should be performed directly, and we have looked exclusively for data on this in randomized clinical trials. when done correctly, provide the best data. We included six studies with 510 patients in this review. The number of patients included in the studies ranged from 40%.
It is positioned so that the drainage holes are both before and after the obstacle. Thus, bile enters the drainage tube before the obstruction and exits from the holes into the intestine after it.
For the first 2-3 days, a plastic bag is connected to the outer end of the drainage (in the intercostal space). This allows you to eliminate excess bile in the ducts and control (detect in time) possible complications, such as hemobilia - bleeding into the bile ducts.
All trials were at high risk of bias, meaning trials may overestimate benefits and underestimate risks. That n there were no significant differences between the two groups in the level of risk of death. The rate of serious complications is higher in patients who have undergone preoperative biliary drainage than among those who work directly. None of the studies reported quality of life, there was no significant difference between the two groups during hospital stay, and none of the studies reported costs. The best evidence currently available does not justify the routine use of a biliary drain before major surgery in patients with biliary obstruction.
If the obstacle cannot be passed, then the drainage is left only to the external outflow in order to reduce the level of bilirubin in the blood and its toxic effects. In such cases, the patient has to drink bile (along with juice or water), since the necessary fluid and trace elements are lost with it, which are necessary for an already depleted body. After a few days, when the inflammation and swelling of the bile duct wall subsides, as a rule, a second attempt is made to pass the obstacle. Once the drain is placed in the desired position, it is fixed to the skin with a suture, which reduces the risk of its displacement.
Regular biliary drainage should not be funded and may lead to litigation. It may also be necessary to conduct well-designed trials with a low risk of systematic errors and random errors. There is currently insufficient evidence to support or avoid routine preoperative biliary drainage in patients with obstructive jaundice. Preoperative biliary drainage may increase the incidence of serious side effects. Thus, the safety of routine preoperative biliary drainage has not been established.
Treatment after a decrease in the level of bilirubin. Care of the drainage of the bile ducts.
 The success of drainage largely depends on the availability of the entire range of instruments in the hospital and the experience of the surgeon performing the intervention. In our department, the success of external-internal drainage with the restoration of the normal passage of bile into the intestine is 98-99%.
The success of drainage largely depends on the availability of the entire range of instruments in the hospital and the experience of the surgeon performing the intervention. In our department, the success of external-internal drainage with the restoration of the normal passage of bile into the intestine is 98-99%.
Preoperative biliary drainage should not be used in patients requiring obstructive surgery for jaundice outside of randomized clinical trials. Patients with obstructive jaundice undergo various pathophysiological changes that affect the liver, kidneys, heart, and immune system. There is considerable controversy regarding the potential benefit to the patient of temporary removal of biliary obstruction prior to the final major surgical procedure.
To assess the benefits and risks of preoperative bile drainage versus preoperative non-bial drainage in patients with obstructive jaundice. Document search strategy. We included all randomized clinical trials comparing surgical operation obstructive jaundice with or without preoperative bile drainage, regardless of size, language, and publication status.
In the case when, after a decrease in the level of bilirubin in the blood, it is possible to carry out a radical surgical intervention (i.e., completely eliminating the root cause of obstructive jaundice), the drainage is removed during or after this operation. In cases where the process is inoperable, the drainage is blocked after a few days and remains with the patient on an ongoing basis. It must be washed - daily once a day, by introducing 20 ml of saline into the drainage. This is done in order to avoid its rapid "blockage" with bile salts or the so-called "sludge" - thick stagnant bile. Patients are prescribed medications that “thinn” bile, such as Ursosan. Despite all these measures, drainage has to be changed every 4-6 months. This happens quite quickly, since there is no need for repeated puncture of the bile ducts and the drainage channel has already been formed.
However, even the very presence of a foreign body in a patient for a long time, even if it is a thin plastic tube without a bag, causes psychological discomfort and reduces the quality of life. By itself, the drainage can be displaced, cause inflammation when food enters through its openings from the intestine into the bile ducts; possible "leakage" of bile through the external drainage channel and soiling clothes.
Stenting of the bile ducts in obstructive jaundice.
In order to avoid these complications, in patients with an inoperable malignant process (in some cases and with other causes of obstructive jaundice), a bile duct stenting operation was developed. In fact, it is a logical continuation of the drainage operation, and, if possible, is performed by a stable patient with a satisfactory prognosis for survival.
Stenting of the bile ducts is usually carried out 1-4 weeks after the drainage operation, after assessing the dynamics of reducing the level of bilirubin and preparing the patient. It is performed through the same access - a thin conductor is inserted into the intestine through the existing drainage, after which the drainage tube is removed. A special balloon is inserted along this conductor, which is positioned inside the stricture (benign or malignant), and opened for a minute for “plasty” of the common bile duct - i.e. expanding it for the possibility of inserting a mesh metal structure into it - a stent.
The diameter of the opened balloon is 6-8mm. The balloon is deflated and removed, and a stent is inserted through the same wire.


The size of the stent is determined in advance, according to the performed cholangiography. Most modern stents are coated with a special material (it looks like fabric from the outside). Such stents are called "grafts" and have a much lower percentage of "tumor growth" through it - and hence the recurrence of obstructive jaundice.
The stent (like the balloon) is rolled up on a special delivery system, which is thin enough and does not require additional expansion of the channel in which the drain was previously located.
The stent is wound and opened in such a way as to close the stricture, but not to block the remaining bile ducts.

If necessary, at the time of opening the balloon and stent, the addition of intravenous anesthesia is used. After the installation of the stent, the patient is observed for several days in the conditions of the surgical department, then, after making sure that there are no complications, they are discharged to continue treatment (chemotherapy, radiation therapy, photodynamic therapy) in a specialized institution or at the place of residence (symptomatic therapy).
Obstructive jaundice is the price of an operation where drainage and stenting of the bile ducts are done.
In most hospitals in St. Petersburg, minimally invasive operations are performed for a fee, because. require rather expensive consumables and the availability of experienced specialists. The City Hospital No. 40 provides residents of St. Petersburg with the opportunity to perform such operations free of charge, according to quotas for high-tech specialized medical care under the Compulsory Medical Insurance program.
Many diseases of the gallbladder and its surrounding organs, such as cholelithiasis and tumors, can cause compression of the ducts. This leads to a violation of the flow of bile into the intestinal cavity and the occurrence of obstructive jaundice. Effective way to stop this formidable condition for health and life, is the surgical drainage of the gallbladder and ducts.
Mechanical or in other words subhepatic jaundice is a serious complication of diseases of the digestive tract and abdominal cavity and a direct indication for drainage of the gallbladder. The pathological process consists in a violation of the outflow of bile from the bladder into the lumen of the duodenum. This leads to an increase in the content of bilirubin in the blood and, as a result, to intoxication of the body.
Subhepatic jaundice can occur at any age and be both benign and malignant.
The most common mechanical obstruction due to tumors and cholelithiasis.
In the video, the doctor talks about common diseases of the gallbladder, methods of treatment and the consequences of pathologies.
Types of drainage
In the vast majority of cases, a special type of surgical intervention is used to temporarily or permanently eliminate symptoms - drainage of the biliary tract and bladder.
There are the following types of this surgical intervention:
- External - the outflow of bladder contents occurs through specially installed conductors to an external receiver.
- External-internal - most of the bile enters the intestine through the channel formed by the doctor, and the remaining contents go to the external receiver.
- Internal drainage - with it, an endoprosthesis of the duct is surgically formed, which ensures the normal passage of bile.
The choice of treatment method depends on the nature of the pathological process, age, concomitant diseases and the state of the patient's cardiovascular system.
It is one of the methods of preparing patients for further surgery. The intervention is low-traumatic, does not require special training and can be performed in any group of patients.
The advantages of this technique include the ability to control the flow of bladder contents, pus and blood. Through the catheter, it is possible to wash the cystic cavity and ducts with antiseptic solutions in order to eliminate the inflammatory process. Through the surgical access, carried out for the installation of drainage, it is also possible to remove stones, as well as excise the scars narrowing the lumen of the ducts.
Contraindications to the method are:
- Violation of blood clotting, a decrease in the level of platelets below 50 g / l.
- Ascites, severe liver failure.
- Extensive, multiple metastases of a malignant neoplasm.
- The presence of hypervascular tumors of the liver in the way of the catheter.
After performing a surgical intervention, constant monitoring of the drainage tube is necessary. The catheter should be flushed with a mixture of saline with novocaine and heparin on the first day.
In the following days, 20 ml of saline is injected daily into the drainage lumen in order to remove clots and prevent obstruction. After stopping the acute period and improving the general condition, doctors can carry out the next stage of the operation, aimed at restoring the normal passage of bladder contents into the intestine.
Patients who underwent external drainage of the biliary tract should periodically undergo examination, determine the level of bilirubin and blood electrolytes. The removal of large amounts of bile from the body can lead to hyponatremia and deterioration of the general condition.
External-internal and internal drainage
Internal drainage of the bile ducts is performed as a palliative treatment for patients with advanced oncopathology. In this case, a permanent endoprosthesis is installed, which ensures the normal flow of bile into the intestinal cavity.
The external-internal type of drainage is recognized as the most effective. With this type of operation, it remains possible to control the patency of the tube, flush the drainage with antiseptic solutions. In addition, most of the bile is not excreted, but enters the duodenum through a special anastomosis, thereby preventing the occurrence of electrolyte disturbances.
The catheter can be placed endoscopically as well as by percutaneous transhepatic drainage. The choice of technique depends on the localization of the pathological process that caused the violation of the outflow of bile.
Thanks to this surgical intervention, it is possible to better prepare the patient for the main operation (removal of stones, tumors), and in the case of palliative treatment, to extend the life of patients up to 1 year.
How is the operation performed
Surgical external drainage of the choledochus is a simple procedure, the duration of which is on average 1.5-2 hours. Special preparation is not required, the procedure can be performed both on an emergency basis and as planned.

The operation is performed in several stages:
- On the eve of the planned intervention, it is necessary to pass a general blood test and a coagulogram to assess the blood coagulation system.
- On the day of surgery, planned patients are prescribed antibiotic therapy to prevent infectious complications. During the intervention itself, the patient remains conscious. Painkillers and sedatives enter the blood through an installed venous catheter.
- Installation of drainage is carried out in the conditions of an X-ray room. After the patient is on the operating table, a device will be connected to it that controls blood pressure, pulse and other vital signs, and contrast will be introduced to better visualize the area of operation.
- Under the control of the X-ray image obtained on the screen after the injection of a contrast agent, the surgeon injects a local anesthetic solution into the liver area, after which a catheter is inserted through a small incision to the blocked biliary tract, above the obturation site.
- The catheter is flushed with sterile saline free end is brought out, sutured to the skin and connected to a special bag for receiving bile.
- After this procedure, the patient is transferred to the ward for further observation.
With indications for the installation of internal drainage during the intervention, in addition to the drainage tube that leads the bile out, an endoprosthesis is installed in the duodenum to ensure the outflow of bile from the choledochus, above the site of its blockage by the stone. In the future, the temporary tube through which the bile flows outward is removed, and the outflow of the contents occurs along the engrafted endoprosthesis.
Permanent drains are made of metal, polyethylene and other nonreactive polymers. Specialists prefer metal prostheses, because they have a longer service life.
The success of the operation largely depends on the diagnosed pathology, the place of narrowing of the common bile duct and averages 90%. The rest of the patients manage to achieve partial decompression, which also significantly improves their quality of life.





